Microaggressions: Prevalence and Perspectives of Residents and Fellows in Post-Graduate Medical Education in Kuwait
Affiliations
Affiliations
- Surgery Department, Amiri Hospital, Kuwait City, Kuwait.
- Medical Student, University of Glasgow School of Medicine, Dentistry and Nursing, Glasgow, United Kingdom.
Abstract
Objective: Microaggression prevalence in post-graduate medical education is unknown in Kuwait. The objective is to determine the prevalence of and capture the perspectives on microaggression among post-graduate trainees in Kuwait.
Materials and methods: This is a cross-sectional study of an anonymous online survey targeting residents and fellows in Kuwait. Data collected included demographics, level of training, country of training, microaggression experience, types, and response. Univariate and multivariate analyses were performed using the Chi-square test and binary logistic regression, respectively.
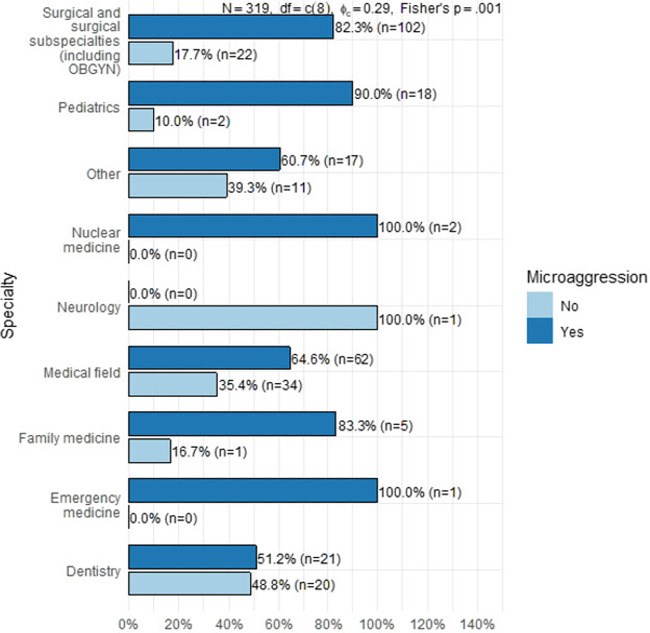
Results: A total of 319 participants (69.1% females) included 52% junior residents, 39.2% senior residents, and 8.78% fellows. Forty-three percent were aware of the microaggression definition. The percentage was significantly higher in respondents from Gulf/Middle East Countries (57.9%) than from Kuwait. Approximately three-quarters experienced microaggressions. Senior residents were more likely to report exposure to microaggressions [Odds ratio (OR) = 2.4, P < 0.05] and had higher odds of exposure than juniors (OR = 9.85, P < 0.05). Exposure to microaggressions was highest in surgery/surgical specialties. The most common act of microaggression was verbal, followed by invalidation/dismissal of thoughts/ideas, and then acts of discrimination. Of those who experienced microaggressions, two-thirds thought that the experience had a psychological effect on them. Both groups reported low confidence in dealing with microaggressions (Gulf/Middle East Countries 18.8% and Kuwait 30.1%); the difference was not statistically significant.
Conclusions: Microaggressions are common among post-graduate medical trainees in Kuwait. Implementation of strategies to manage it is necessary. Further research on its impact on medical-training outcomes is needed.
Keywords: Kuwait; fellows; microaggressions; post-graduate medical education; prevalence; residents; surgery; training.
Conflict of interest statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Figures
Similar articles
Brooks JT, Porter SE, Middleton KK, Carson EW, Ode GE.Clin Orthop Relat Res. 2023 Apr 1;481(4):675-686. doi: 10.1097/CORR.0000000000002455. Epub 2022 Nov 7.PMID: 36342502
Brown C, Daniel R, Addo N, Knight S.AEM Educ Train. 2021 Sep 29;5(Suppl 1):S49-S56. doi: 10.1002/aet2.10670. eCollection 2021 Sep.PMID: 34616973 Free PMC article.
Microaggressions and Implicit Bias in Surgical Training: An Undocumented but Pervasive Phenomenon.
Alimi Y, Bevilacqua LA, Snyder RA, Walsh D, Jackson PG, DeMaria EJ, Tuttle JE, Altieri MS.Ann Surg. 2023 Jan 1;277(1):e192-e196. doi: 10.1097/SLA.0000000000004917. Epub 2021 Apr 9.PMID: 33843793
Understanding and Addressing Microaggressions in Medicine.
Weir M.Dermatol Clin. 2023 Apr;41(2):291-297. doi: 10.1016/j.det.2022.08.006. Epub 2023 Feb 1.PMID: 36933918 Review.
A Scoping Review of Recommendations and Training to Respond to Patient Microaggressions.
Wittkower LD, Bryan JL, Asghar-Ali AA.Acad Psychiatry. 2022 Oct;46(5):627-639. doi: 10.1007/s40596-021-01533-9. Epub 2021 Oct 6.PMID: 34613599 Review.
KMEL References
References
-
- Solorzano D, Ceja M, Yosso T. Critical race theory, racial microaggressions, and campus racial climate: the experiences of African American college students. J Negro Educ. (2000) 69(1/2):60.
-
- Nadal KL, Wong Y, Griffin KE, Davidoff K, Sriken J. The adverse impact of racial microaggressions on college students’ self-esteem. J Coll Stud Dev. (2014) 55(5):461–74. 10.1353/csd.2014.0051 - DOI
-
- Nadal KL, Griffin KE, Wong Y, Hamit S, Rasmus M. The impact of racial microaggressions on mental health: Counseling implications for clients of color. J Couns Dev. (2014) 92(1):57–66. 10.1002/j.1556-6676.2014.00130.x - DOI
-
- Forrest-Bank SS, Cuellar MJ. The mediating effects of ethnic identity on the relationships between racial microaggression and psychological well-being. Soc Work Res. (2018) 42(1):44–56. 10.1093/swr/svx023 - DOI
-
- Martin JL. Microaggression Theory influence and implications. In: Torino GC, Rivera DP, Capodilupo CM, Nadal KL, Sue DW, editors. Factors Contributing to Microaggressions, Racial Battle Fatigue, Stereotype Threat, and Imposter Phenomenon for Nonhegemonic Students: Implications for Urban Education. Wiley; (2018). p. 102–20. Available from: https://onlinelibrary.wiley.com/doi/10.1002/9781119466642.ch7 [cited 2022 March].
-
- Al Rashed A, AlShemeri F. Attitudes and barriers towards pursuing a surgical specialty in medical students and interns in Kuwait: A cross-sectional study. Surg Pract Sci. (2022) 8(1). 10.1016/j.sipas.2022.100060 - DOI
-
- Al-Rashed A, Al-Gilani M. Gender Equity in Surgical Academia in Kuwait and the Arabian Gulf Region. In: Bellini M, Papalois V, editors. Gender Equity in the Medical Profession. IGI Global; (2020). p. 237–51.
-
- American College of Surgeons. Managing Microaggressions: What to Do When It Gets Personal Webinar Series - Part 2. Jun 21, 2021. Accessed March 25, 2022.