Acceptance of COVID-19 Vaccine Booster Doses Using the Health Belief Model: A Cross-Sectional Study in Low-Middle- and High-Income Countries of the East Mediterranean Region
Ramy Mohamed Ghazy 1, Marwa Shawky Abdou 2, Salah Awaidy 3, Malik Sallam 4 5 6, Iffat Elbarazi 7, Naglaa Youssef 8, Osman Abubakar Fiidow 9, Slimane Mehdad 10, Mohamed Fakhry Hussein 11, Mohammed Fathelrahman Adam 12, Fatimah Saed Alabd Abdullah 13, Wafa Kammoun Rebai 14, Etwal Bou Raad 15 16, Mai Hussein 17 18, Shehata F Shehata 19 20, Ismail Ibrahim Ismail 21, Arslan Ahmed Salam 22, Dalia Samhouri 23
Affiliations
Affiliations
- Tropical Health Department, High Institute of Public Health, Alexandria University, Alexandria 21561, Egypt.
- 2Department of Epidemiology, High Institute of Public Health, Alexandria University, Alexandria 21561, Egypt.
- 3Health Affairs, Ministry of Health, Muscat 100, Oman.
- 4Department of Pathology, Microbiology and Forensic Medicine, School of Medicine, The University of Jordan, Amman 11942, Jordan.
- 5Department of Clinical Laboratories and Forensic Medicine, Jordan University Hospital, Amman 11942, Jordan.
- 6Department of Translational Medicine, Faculty of Medicine, Lund University, 22184 Malmö, Sweden.
- 7Institute of Public Health, College of Medicine and Health Sciences, United Arab Emirates University, AlAin 15551, United Arab Emirates.
- 8Department of Medical-Surgical Nursing, College of Nursing, Princess Nourah bint Abdulrahman University, Riyadh 11671, Saudi Arabia.
- 9School of Public Health and Research, Somali National University, Mogadishu P.O. Box 15, Somalia.
- 10Physiology and Physiopathology Research Team, Research Centre of Human Pathology Genomics, Faculty of Sciences, Mohammed V University, Rabat BP 8007, Morocco.
- 11Occupational Health and Industrial Medicine Department, High Institute of Public Health, Alexandria University, Alexandria 21526, Egypt.
- 12Faculty of Pharmacy, University of Science and Technology, Khartoum P.O. Box 12810, Sudan.
- 13Internal Medicine Department, Faculty of Medicine, Alexandria University, Alexandria 21526, Egypt.
- 14Institute Pasteur de Tunis, Tunis 2092, Tunisia.
- 15Department of Epidemiology and Population Health, American University of Beirut, Beirut P.O. Box 110236, Lebanon.
- 16School of Pharmacy, Lebanese International University, Beirut P.O. Box 146404, Lebanon.
- 17Clinical Research Administration, Alexandria Directorate of Health Affairs, Egyptian Ministry of Health and Population, Alexandria 21554, Egypt.
- 18Harvard Medical School, Boston, MA 02115, USA.
- 19Department of Family and Community Medicine, King Khalid University, Abha 62529, Saudi Arabia.
- 20Biostatistics Department, High Institute of Public Health, Alexandria University, Alexandria 21561, Egypt.
- 21Department of Neurology, Ibn Sina Hospital, Gamal Abdel Nasser Street, Sabah Medical Area, Safat 070001, Kuwait.
- 22National Institute of Health, Islamabad 45320, Pakistan.
- 23Emergency Preparedness and International Health Regulations, WHO EMRO (DS), P.O. Box 7608, Naser City 11371, Egypt.
Abstract
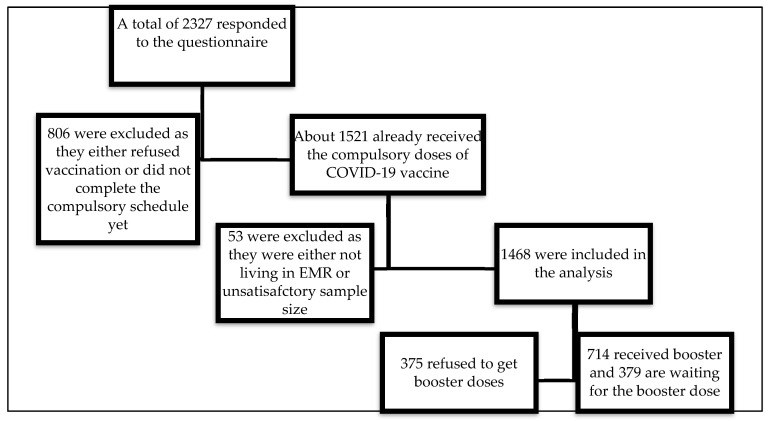
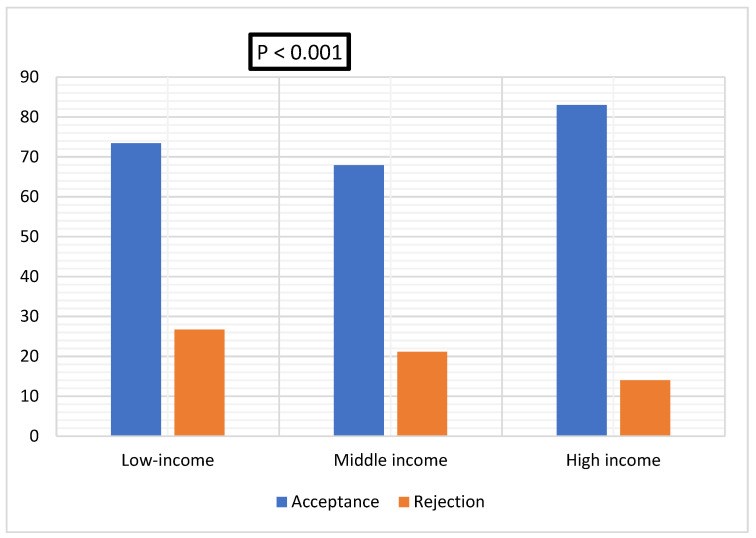
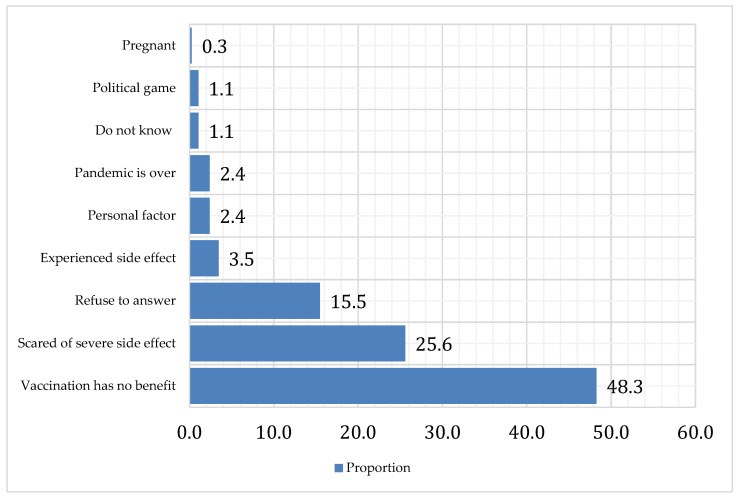
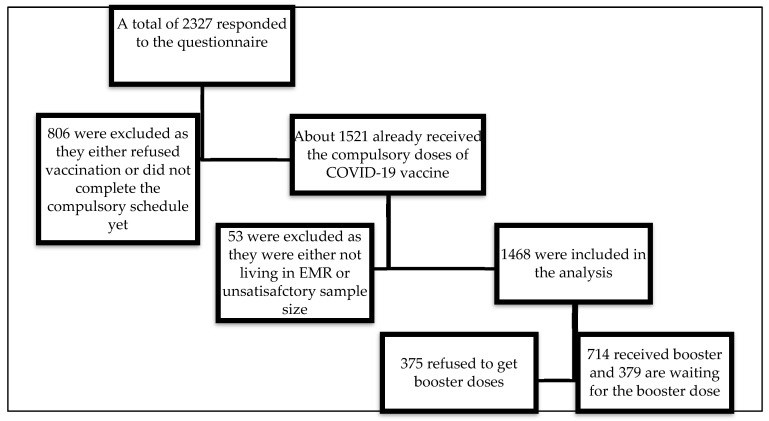
Coronavirus disease (COVID-19) booster doses decrease infection transmission and disease severity. This study aimed to assess the acceptance of COVID-19 vaccine booster doses in low, middle, and high-income countries of the East Mediterranean Region (EMR) and its determinants using the health belief model (HBM). In addition, we aimed to identify the causes of booster dose rejection and the main source of information about vaccination. Using the snowball and convince sampling technique, a bilingual, self-administered, anonymous questionnaire was used to collect the data from 14 EMR countries through different social media platforms. Logistic regression analysis was used to estimate the key determinants that predict vaccination acceptance among respondents. Overall, 2327 participants responded to the questionnaire. In total, 1468 received compulsory doses of vaccination. Of them, 739 (50.3%) received booster doses and 387 (26.4%) were willing to get the COVID-19 vaccine booster doses. Vaccine booster dose acceptance rates in low, middle, and high-income countries were 73.4%, 67.9%, and 83.0%, respectively (p < 0.001). Participants who reported reliance on information about the COVID-19 vaccination from the Ministry of Health websites were more willing to accept booster doses (79.3% vs. 66.6%, p < 0.001). The leading causes behind booster dose rejection were the beliefs that booster doses have no benefit (48.35%) and have severe side effects (25.6%). Determinants of booster dose acceptance were age (odds ratio (OR) = 1.02, 95% confidence interval (CI): 1.01-1.03, p = 0.002), information provided by the Ministry of Health (OR = 3.40, 95% CI: 1.79-6.49, p = 0.015), perceived susceptibility to COVID-19 infection (OR = 1.88, 95% CI: 1.21-2.93, p = 0.005), perceived severity of COVID-19 (OR = 2.08, 95% CI: 137-3.16, p = 0.001), and perceived risk of side effects (OR = 0.25, 95% CI: 0.19-0.34, p < 0.001). Booster dose acceptance in EMR is relatively high. Interventions based on HBM may provide useful directions for policymakers to enhance the population's acceptance of booster vaccination.
Keywords: COVID-19 vaccine; East Mediterranean region; booster dose acceptance; health belief model; vaccine hesitancy.
Conflict of interest statement
The authors declare no conflict of interest.
Figures
Similar articles
Qin C, Yan W, Du M, Liu Q, Tao L, Liu M, Liu J.Front Public Health. 2022 Dec 15;10:986916. doi: 10.3389/fpubh.2022.986916. eCollection 2022.PMID: 36589991 Free PMC article.
Qin C, Wang R, Tao L, Liu M, Liu J.Front Public Health. 2022 Mar 16;10:834572. doi: 10.3389/fpubh.2022.834572. eCollection 2022.PMID: 35372197 Free PMC article.
Roy DN, Azam MS, Islam E.PLoS One. 2023 Apr 13;18(4):e0281395. doi: 10.1371/journal.pone.0281395. eCollection 2023.PMID: 37053270 Free PMC article.
COVID-19 Vaccine Booster Dose Acceptance: Systematic Review and Meta-Analysis.
Abdelmoneim SA, Sallam M, Hafez DM, Elrewany E, Mousli HM, Hammad EM, Elkhadry SW, Adam MF, Ghobashy AA, Naguib M, Nour El-Deen AE, Aji N, Ghazy RM.Trop Med Infect Dis. 2022 Oct 13;7(10):298. doi: 10.3390/tropicalmed7100298.PMID: 36288039 Free PMC article. Review.
Hong J, Xu XW, Yang J, Zheng J, Dai SM, Zhou J, Zhang QM, Ruan Y, Ling CQ.J Integr Med. 2022 Jan;20(1):34-44. doi: 10.1016/j.joim.2021.10.004. Epub 2021 Oct 26.PMID: 34774463 Free PMC article. Review.
Cited by
Ghazy RM, Sallam M, Abdullah FSA, Hussein M, Hussein MF.J Epidemiol Glob Health. 2023 May 12:1-11. doi: 10.1007/s44197-023-00107-2. Online ahead of print.PMID: 37171545 Free PMC article.
Limbu YB, Gautam RK.Vaccines (Basel). 2023 Apr 7;11(4):816. doi: 10.3390/vaccines11040816.PMID: 37112728 Free PMC article. Review.
Fadl N, Al Awaidy ST, Elshabrawy A, Makhlouf MSAH, Ibrahim SA, Abdel-Rahman S, Tookhy NA, Alsalmani A, Al-Saeedi M, Al-Sawalha I, El-Din MAA, Saad J, Ayoob Z, Rourou MK, Ali M, Tawati SM, Gadain YMA, Al-Saidi SY, Hassan GA, Alsanafi M, Sandouk L, Youssef N, Alothman S, Yazbek S, Al-Ansi KS, Mehdad S, Adam MF, Gebreal A, Ghazy RM.Front Public Health. 2023 Mar 28;11:1132798. doi: 10.3389/fpubh.2023.1132798. eCollection 2023.PMID: 37056660 Free PMC article.
COVID-19 Vaccine Booster Hesitancy in Malaysia: A Web-Based Cross-Sectional Study.
Lee KW, Yap SF, Ong HT, Oo M, Swe KMM.Vaccines (Basel). 2023 Mar 13;11(3):638. doi: 10.3390/vaccines11030638.PMID: 36992222 Free PMC article.
Why Some People Are Hesitant to Receive COVID-19 Boosters: A Systematic Review.
Limbu YB, Huhmann BA.Trop Med Infect Dis. 2023 Mar 5;8(3):159. doi: 10.3390/tropicalmed8030159.PMID: 36977160 Free PMC article. Review.
KMEL References
References
-
- World Health Organization WHO Coronavirus (COVID-19) Dashboard. [(accessed on 19 September 2022)]; Available online: https://covid19.who.int/
-
- Lang R., Atabati O., Oxoby R.J., Mourali M., Shaffer B., Sheikh H., Fullerton M.M., Tang T., Leigh J.P., Manns B.J., et al. Characterization of non-adopters of COVID-19 non-pharmaceutical interventions through a national cross-sectional survey to assess attitudes and behaviours. Sci. Rep. 2021;11:21751. doi: 10.1038/s41598-021-01279-2. - DOI - PMC - PubMed
-
- Bo Y., Guo C., Lin C., Zeng Y., Li H.B., Zhang Y., Hossain M.S., Chan J.W.M., Yeung D.W., Kwok K.O., et al. Effectiveness of non-pharmaceutical interventions on COVID-19 transmission in 190 countries from 23 January to 13 April 2020. Int. J. Infect. Dis. 2021;102:247–253. doi: 10.1016/j.ijid.2020.10.066. - DOI - PMC - PubMed
-
- World Health Organization WHO Coronavirus (COVID-19) Dashboard. [(accessed on 14 September 2022)]; Available online: https://covid19.who.int/?mapFilter=vaccinations.
-
- Alishaq M., Nafady-Hego H., Jeremijenko A., Al Ajmi J.A., Elgendy M., Vinoy S., Fareh S.B., Veronica Plaatjies J., Nooh M., Alanzi N. Risk factors for breakthrough SARS-CoV-2 infection in vaccinated healthcare workers. PLoS ONE. 2021;16:e0258820. doi: 10.1371/journal.pone.0258820. - DOI - PMC - PubMed
-
- Vicenti I., Basso M., Gatti F., Scaggiante R., Boccuto A., Zago D., Modolo E., Dragoni F., Parisi S.G., Zazzi M. Faster decay of neutralizing antibodies in never infected than previously infected healthcare workers three months after the second BNT162b2 mRNA COVID-19 vaccine dose. Int. J. Infect. Dis. 2021;112:40–44. doi: 10.1016/j.ijid.2021.08.052. - DOI - PMC - PubMed
-
- Yue L., Zhou J., Zhou Y., Yang X., Xie T., Yang M., Zhao H., Zhao Y., Yang T., Li H. Antibody response elicited by a third boost dose of inactivated SARS-CoV-2 vaccine can neutralize SARS-CoV-2 variants of concern. Emerg. Microbes Infect. 2021;10:2125–2127. doi: 10.1080/22221751.2021.1996210. - DOI - PMC - PubMed
-
- Goren A., Cadegiani F.A., Warmbier C.G., Vano-Galvan S., Tosti A., Shapiro J., Mesinkovska N.A., Ramos P.M., Sinclair R., Lupi O. Androgenetic alopecia may be associated with weaker COVID-19 T-cell immune response: An insight into a potential COVID-19 vaccine booster. Med. Hypotheses. 2021;146:110439. doi: 10.1016/j.mehy.2020.110439. - DOI - PMC - PubMed
-
- Fajar J.K., Sallam M., Soegiarto G., Sugiri Y.J., Anshory M., Wulandari L., Kosasih S.A.P., Ilmawan M., Kusnaeni K., Fikri M., et al. Global Prevalence and Potential Influencing Factors of COVID-19 Vaccination Hesitancy: A Meta-Analysis. Vaccines. 2022;10:1356. doi: 10.3390/vaccines10081356. - DOI - PMC - PubMed
-
- ElSayed D.A., Bou Raad E., Bekhit S.A., Sallam M., Ibrahim N.M., Soliman S., Abdullah R., Farag S., Ghazy R.M. Validation and Cultural Adaptation of the Parent Attitudes about Childhood Vaccines (PACV) Questionnaire in Arabic Language Widely Spoken in a Region with a High Prevalence of COVID-19 Vaccine Hesitancy. Trop. Med. Infect. Dis. 2022;7:234. doi: 10.3390/tropicalmed7090234. - DOI - PMC - PubMed
-
- World Health Organization Ten Threats to Global Health in 2019. [(accessed on 14 September 2022)]; Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-....
-
- World Health Organization Health Inequities in the Eastern Mediterranean Region: Selected Country Case Studies. [(accessed on 16 September 2022)]; Available online: https://apps.who.int/iris/handle/10665/204666.
-
- Abdou M.S., Kheirallah K.A., Aly M.O., Ramadan A., Elhadi Y.A.M., Elbarazi I., Deghidy E.A., El Saeh H.M., Salem K.M., Ghazy R.M. The coronavirus disease 2019 (COVID-19) vaccination psychological antecedent assessment using the Arabic 5c validated tool: An online survey in 13 Arab countries. PLoS ONE. 2021;16:e0260321. doi: 10.1371/journal.pone.0260321. - DOI - PMC - PubMed
-
- Rababa’h A., Abedalqader N., Ababneh M. Jordanians’ willingness to receive heterologous prime-boost COVID-19 vaccination and vaccine boosters. Eur. Rev. Med. Pharmacol. Sci. 2021;25:7516–7525. - PubMed
-
- Patwary M.M., Bardhan M., Disha A.S., Hasan M., Haque M.Z., Sultana R., Hossain M.R., Browning M.H.E.M., Alam M.A., Sallam M. Determinants of COVID-19 Vaccine Acceptance among the Adult Population of Bangladesh Using the Health Belief Model and the Theory of Planned Behavior Model. Vaccines. 2021;9:1393. doi: 10.3390/vaccines9121393. - DOI - PMC - PubMed
-
- Bandura A., Freeman W.H., Lightsey R. Self-Efficacy: The Exercise of Control. J. Cogn. Psychother. 1999;13 doi: 10.1891/0889-8391.13.2.158. - DOI
-
- Abouzid M., Ahmed A.A., El-Sherif D.M., Alonazi W.B., Eatmann A.I., Alshehri M.M., Saleh R.N., Ahmed M.H., Aziz I.A., Abdelslam A.E., et al. Attitudes toward Receiving COVID-19 Booster Dose in the Middle East and North Africa (MENA) Region: A Cross-Sectional Study of 3041 Fully Vaccinated Participants. Vaccines. 2022;10:1270. doi: 10.3390/vaccines10081270. - DOI - PMC - PubMed
-
- Wang H., Huang Y.-M., Su X.-Y., Xiao W.-J., Si M.-Y., Wang W.-J., Gu X.-F., Ma L., Li L., Zhang S.-K. Acceptance of the COVID-19 vaccine based on the health belief model: A multicenter national survey among medical care workers in China. Hum. Vaccines Immunother. 2022;18:2076523. doi: 10.1080/21645515.2022.2076523. - DOI - PMC - PubMed
-
- Ai J., Zhang Y., Zhang H., Zhang Q., Fu Z., Lin K., Song J., Zhao Y., Fan M., Wang H. Safety and immunogenicity of a third-dose homologous BBIBP-CorV boosting vaccination: Interim results from a prospective open-label study. Emerg. Microbes Infect. 2022;11:639–647. doi: 10.1080/22221751.2022.2025746. - DOI - PMC - PubMed
-
- Ashmawy R., Hamdy N.A., Elhadi Y.A.M., Alqutub S.T., Esmail O.F., Abdou M.S.M., Reyad O.A., El-Ganainy S.O., Gad B.K., Nour El-Deen A.E.-S. A Meta-Analysis on the Safety and Immunogenicity of CovId-19 vaccines. J. Prim. Care Community Health. 2022;13:21501319221089255. doi: 10.1177/21501319221089255. - DOI - PMC - PubMed
-
- Moawad A.M., Taha S.H.N., Ghazy R.M., Abdelhalim W.A. Assessment of Self-Treatment Knowledge, Beliefs and Practice during COVID-19 Pandemic among Egyptian Population: A Cross-Sectional Study. Egypt. J. Hosp. Med. 2022;89:4516–4525.
-
- Shaaban R., Ghazy R.M., Elsherif F., Ali N., Yakoub Y., Aly M.O., ElMakhzangy R., Abdou M.S., McKinna B., Elzorkany A.M., et al. COVID-19 Vaccine Acceptance among Social Media Users: A Content Analysis, Multi-Continent Study. Int. J. Environ. Res. Public Health. 2022;19:5737. doi: 10.3390/ijerph19095737. - DOI - PMC - PubMed
-
- Pacific W., Hasan S.A.W. Interim Statement on Booster Doses for COVID-19 Vaccination. WHO; Geneva, Switzerland: 2021. Update.
-
- Jairoun A.A., Al-Hemyari S.S., El-Dahiyat F., Jairoun M., Shahwan M., Al Ani M., Habeb M., Babar Z.-U.-D. Assessing public knowledge, attitudes and determinants of third COVID-19 vaccine booster dose acceptance: Current scenario and future perspectives. J. Pharm. Policy Pract. 2022;15:26. doi: 10.1186/s40545-022-00422-2. - DOI - PMC - PubMed
-
- Patwary M.M., Alam M.A., Bardhan M., Disha A.S., Haque M.Z., Billah S.M., Kabir M.P., Browning M.H., Rahman M.M., Parsa A.D. COVID-19 Vaccine Acceptance among Low-and Lower-Middle-Income Countries: A Rapid Systematic Review and Meta-Analysis. Vaccines. 2022;10:427. doi: 10.3390/vaccines10030427. - DOI - PMC - PubMed
-
- Wang R., Zhang Q., Ge J., Ren W., Zhang R., Lan J., Ju B., Su B., Yu F., Chen P. Analysis of SARS-CoV-2 variant mutations reveals neutralization escape mechanisms and the ability to use ACE2 receptors from additional species. Immunity. 2021;54:1611–1621.e5. doi: 10.1016/j.immuni.2021.06.003. - DOI - PMC - PubMed