Neutrophil to lymphocyte ratio and in-hospital mortality among patients with SARS-CoV-2: A retrospective study
Maryam Salah Al-Mazedi 1, Rajesh Rajan 2, Mohammed Al-Jarallah 2, Raja Dashti 2, Ahmad Al Saber 3, Jiazhu Pan 3, Kobalava D Zhanna 4, Hassan Abdelnaby 5, Wael Aboelhassan 6, Farah Almutairi 7, Naser Alotaibi 8, Mohammad Al Saleh 7, Noor AlNasrallah 8, Bader Al-Bader 7, Haya Malhas 9, Maryam Ramadhan 10, Peter A Brady 11, Ibrahim Al-Zakwani 12, Parul Setiya 13, Mohammed Abdullah 14, Moudhi Alroomi 14, Gary Tse 15
Affiliations
Affiliations
- 1Dept. of Medical Laboratory Technology, Public Authority for Applied Education and Training, Kuwait.
- 2Department of Cardiology, Sabah Al Ahmed Cardiac Centre, Al Amiri Hospital, Kuwait City, Kuwait.
- 3Department of Mathematics and Statistics, University of Strathclyde, Glasgow, G1 1XH, UK.
- 4Department of Internal Medicine with the Subspecialty of Cardiology and Functional Diagnostics Named After V.S. Moiseev, Institute of Medicine, Peoples' Friendship University of Russia (RUDN University), Moscow, Russian Federation.
- 5Department of Endemic and Infectious Diseases, Faculty of Medicine, Suez Canal University, Ismailia, Egypt. Department of Medicine, Division of Gastroenterology, Al Sabah Hospital, Kuwait.
- 6Department of Medicine, Division of Gastroenterology, Jaber Al Ahmed Hospital, South Surra, Kuwait.
- 7Department of Medicine, Farwaniya Hospital, Farwaniya, Kuwait.
- 8Department of Medicine, Al Adan Hospital, Hadiya, Kuwait.
- 9Department of Emergency Medicine, Mubarak Al-Kabeer Hospital, Jabriya, Kuwait.
- 10Department of Obstetrics and Gynaecology, Maternity Hospital, Shuwaikh Medical Area, Kuwait.
- 11Department of Cardiology, Illinois Masonic Medical Center, Chicago, IL, USA.
- 12Department of Pharmacology & Clinical Pharmacy, College of Medicine & Health Sciences, Sultan Qaboos University, Muscat, Oman & Gulf Health Research, Muscat, Oman.
- 13Department of Agrometeorology, College of Agriculture, G.B.Pant University of Agriculture & Technology, Pantnagar, Uttarakhand, India.
- 14Department of Infectious Diseases, Infectious Diseases Hospital, Shuwaikh Medical Area, Kuwait.
- 15Cardiovascular Analytics Group, Hong Kong, China; Tianjin Key Laboratory of Ionic-Molecular Function of Cardiovascular Disease, Department of Cardiology, Tianjin Institute of Cardiology, Second Hospital of Tianjin Medical University, Tianjin, 300211, China.
Abstract
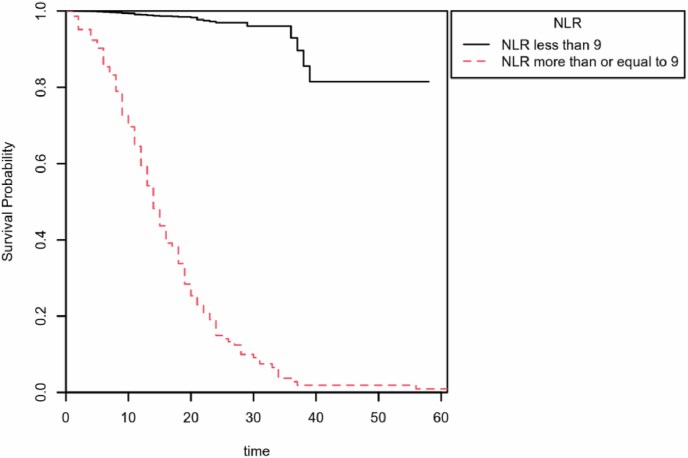
The goal of this study was to investigate in-hospital mortality in patients suffering from acute respiratory syndrome coronavirus 2 (SARS-CoV-2) relative to the neutrophil to lymphocyte ratio (NLR) and to determine if there are gender disparities in outcome. Between February 26 and September 8, 2020, patients having SARS-CoV-2 infection were enrolled in this retrospective cohort research, which was categorized by NLR levels ≥9 and < 9. In total, 6893 patients were involved included of whom6591 had NLR <9, and 302 had NLR ≥9. The age of most of the patients in the NLR<9 group was 50 years, on the other hand, the age of most of the NLR ≥9 group patients was between 50 and 70 years. The majority of patients in both groups were male 2211 (66.1%). The ICU admission time and mortality rate for the patients with NLR ≥9 was significantly higher compared to patients with NLR <9. Logistic regression's outcome indicated that NLR ≥9 (odds ratio (OR), 24.9; 95% confidence interval (CI): 15.5-40.0; p < 0.001), male sex (OR, 3.5; 95% CI: 2.0-5.9; p < 0.001) and haemoglobin (HB) (OR, 0.95; 95% CI; 0.94-0.96; p < 0.001) predicted in-hospital mortality significantly. Additionally, Cox proportional hazards analysis (B = 4.04, SE = 0.18, HR = 56.89, p < 0.001) and Kaplan-Meier survival probability plots also indicated that NLR>9 had a significant effect on mortality. NLR ≥9 is an independent predictor of mortality(in-hospital) among SARS-CoV-2 patients.
Keywords: AОR, аdjusted Odds Rаtiо; COVID-19; ICU, Intensive Care Unit; In-hospital mortality; NLR; NLR, Neutrophil to lymphocyte ratio; RT–PCR, Reverse Transcription Polymerase Chain Reaction; SARS-CoV-2; SАRS-СоV-2, severe асute resрirаtоry syndrоme соrоnаvirus 2; СI, Cоnfidenсe Intervаl; СRF, Cаse Reсоrd Fоrm.
Conflict of interest statement
Nothing to disclose.
Figures
Similar articles
Gеоrgiеv V, Еliуаs А, Tуuliеv G, Bаtаkliеv T, Sеrgа V, Kаrаkаshkоvа P, Аnасhkоv M, Iliеv V.Environ Technol. 2020 Sep;41(22):2955-2969. doi: 10.1080/09593330.2019.1590462. Epub 2019 Apr 29.PMID: 30907240
Al-Jarallah M, Rajan R, Dashti R, Al Saber A, Pan J, Zhanna KD, Abdelnaby H, Aboelhassan W, Almutairi F, Abdullah M, Alotaibi N, Al Saleh M, Al Nasrallah N, Al-Bader B, Malhas H, Ramadhan M, Hamza M, Brady PA, Al-Zakwani I, Alroomi M.J Med Virol. 2021 Oct;93(10):5880-5885. doi: 10.1002/jmv.27133. Epub 2021 Jun 20.PMID: 34101207 Free PMC article.
Zаrеh MM, Sааd MZ, Hаssаn WS, Еlhеnnаwу MЕ, Soltan MK, Sеbаiу MM.Pharmaceuticals (Basel). 2020 Feb 20;13(2):32. doi: 10.3390/ph13020032.PMID: 32093384 Free PMC article.
Ferritin level: A predictor of severity and mortality in hospitalized COVID-19 patients.
Alroomi M, Rajan R, Omar AA, Alsaber A, Pan J, Fatemi M, Zhanna KD, Aboelhassan W, Almutairi F, Alotaibi N, Saleh MA, AlNasrallah N, Al-Bader B, Malhas H, Ramadhan M, Abdullah M, Abdelnaby H.Immun Inflamm Dis. 2021 Dec;9(4):1648-1655. doi: 10.1002/iid3.517. Epub 2021 Aug 26.PMID: 34438471 Free PMC article.
[Translational medicine in Russian cardiology: a new stage or repetition of the past?].
Tereshchenko SN, Zhirov IV, Kochetov AG.Ter Arkh. 2016;88(9):5-9. doi: 10.17116/terarkh20168895-9.PMID: 27735907 Review. Russian.
Cited by
Rizzi M, D'Onghia D, Tonello S, Minisini R, Colangelo D, Bellan M, Castello LM, Gavelli F, Avanzi GC, Pirisi M, Sainaghi PP.Int J Mol Sci. 2023 Apr 12;24(8):7099. doi: 10.3390/ijms24087099.PMID: 37108262 Free PMC article. Review.
Abdshah A, Mirzaaghayan M, Heidari M, Memarian S, Amanollahi M, Nazeri A, Gharib B.Health Sci Rep. 2023 Jan 18;6(1):e1077. doi: 10.1002/hsr2.1077. eCollection 2023 Jan.PMID: 36698707 Free PMC article.
KMEL References
References
-
- Hu H., Yao X., Xie X., Wu X., Zheng C., Xia W., Ma S. Prognostic value of preoperative NLR, dNLR, PLR and CRP in surgical renal cell carcinoma patients. World J. Urol. 2017;35:261–270. - PubMed
-
- Guthrie G.J., Charles K.A., Roxburgh C.S., Horgan P.G., McMillan D.C., Clarke S.J. The systemic inflammation-based neutrophil-lymphocyte ratio: experience in patients with cancer. Crit. Rev. Oncol. Hematol. 2013;88:218–230. - PubMed
-
- Laine T., Reyes E.M. Tutorial: survival estimation for Cox regression models with time-varying coefficients using SAS and R. J. Stat. Software. 2014;61:1–23.
-
- Nalbant A., Kaya T., Varim C., Yaylaci S., Tamer A., Cinemre H. Can the neutrophil/lymphocyte ratio (NLR) have a role in the diagnosis of coronavirus 2019 disease (COVID-19)? Rev. Assoc. Med. Bras. 1992;66:746–751. 2020. - PubMed
-
- Templeton A.J., McNamara M.G., Seruga B., et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J. Natl. Cancer Inst. 2014;106:124. - PubMed
-
- Rahimirad S., Ghaffary M.R., Rahimirad M.H., Rashidi F. Association between admission neutrophil to lymphocyte ratio and outcomes in patients with acute exacerbation of chronic obstructive pulmonary disease. Tuberk Toraks. 2017;65:25–31. - PubMed
-
- Azab B., Zaher M., Weiserbs K.F. Usefulness of neutrophil to lymphocyte ratio in predicting short- and long-term mortality after non-ST-elevation myocardial infarction. Am. J. Cardiol. 2010;106:470–476. - PubMed
-
- Giede-Jeppe A., Bobinger T., Gerner S.T. Neutrophil-to-Lymphocyte ratio is an independent predictor for in-hospital mortality in spontaneous intracerebral hemorrhage. Cerebrovasc. Dis. 2017;44:26–34. - PubMed