Stress Hyperglycemia Ratio as a Prognostic Marker in Diabetic Patients Hospitalized with COVID-19
Mohamed Aon 1, Abdullah Alsaeedi 2, Azeez Alzafiri 2, Abdelrahman Al-Shammari 2, Sherif Taha 1, Omar Al-Shammari 2, Mahmoud Tawakul 2, Jarrah Alshammari 2, Naser Alherz 2, Monerah Alenezi 2, Meshari Eyadah 2, Mariam Aldhafeeri 2, Teflah Alharbi 2, Duaa Alshammari 2, Zaid Alenezi 2, Salem Aldouseri 2, Ebraheem Albazee 2, Mohamed M Ibrahim 3, Ahmed H Aoun 4
Affiliations
Affiliations
- Department of Internal Medicine, Faculty of Medicine, Cairo University, Giza 12613, Egypt.
- Department of Internal Medicine, Jahra Hospital, Jahra 2675, Kuwait.
- Jaber Al-Ahmad Military Hospital, Ministry of Defense, Kuwait City 46001, Kuwait.
- Department of Pediatrics, Faculty of Medicine, Cairo University, Giza 12613, Egypt.
Abstract
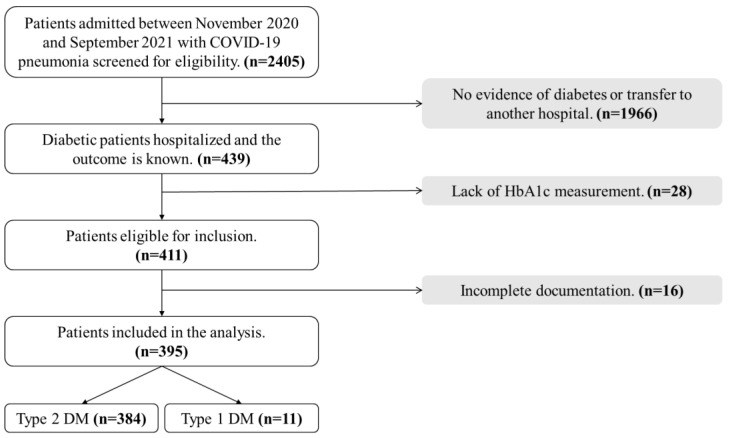
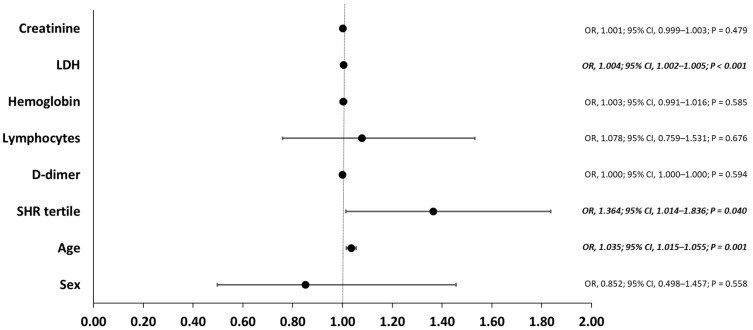
Evidence is conflicting about the diabetes characteristics associated with worse outcome among hospitalized COVID-19 patients. We aimed to assess the role of stress hyperglycemia ratio (SHR) as a prognostic marker among them. In our retrospective cohort study, patients were stratified according to SHR, admission glucose, and glycated hemoglobin tertiles. The primary outcome was a composite endpoint of invasive mechanical ventilation, intensive care unit admission, and in-hospital mortality. The study included 395 patients with a mean age of 59 years, and 50.1% were males. Patients in the third tertile of SHR developed more primary events, and the difference was significant compared to the first tertile (p = 0.038) and close to significance compared to the second tertile (p = 0.054). There was no significant difference in the outcomes across admission glucose and glycated hemoglobin tertiles. A higher SHR tertile was an independent risk factor for the primary outcome (OR, 1.364; 95% CI: 1.014-1.836; p = 0.040) after adjustment for other covariables. In hospitalized COVID-19 diabetic patients, SHR third tertile was significantly associated with worse outcome and death. SHR can be a better prognostic marker compared to admission glucose and glycated hemoglobin. A higher SHR was an independent risk factor for worse outcome and in-hospital mortality.
Keywords: COVID-19; SARS-CoV-2; diabetes mellitus; hyperglycemia; stress hyperglycemia ratio.
Conflict of interest statement
The authors declare no conflict of interest.
Figures
Similar articles
Low stress hyperglycemia ratio predicts worse prognosis in diabetic acute heart failure patients.
Cunha FM, Carreira M, Ferreira I, Bettencourt P, Lourenço P.Rev Port Cardiol. 2023 May;42(5):433-441. doi: 10.1016/j.repc.2022.02.013. Epub 2023 Jan 9.PMID: 36634761 English, Portuguese.
Song Q, Dai M, Zhao Y, Lin T, Huang L, Yue J.BMC Geriatr. 2022 Apr 4;22(1):277. doi: 10.1186/s12877-022-02935-6.PMID: 35369877 Free PMC article.
Matias AA, Manique I, Sabino T, Rego T, Mihon C, Panarra A, Rizzo M, Silva-Nunes J.Diabetes Ther. 2023 Feb;14(2):335-346. doi: 10.1007/s13300-022-01347-4. Epub 2022 Dec 27.PMID: 36574200 Free PMC article.
Koracevic GP.J Emerg Med. 2016 Jul;51(1):31-6. doi: 10.1016/j.jemermed.2015.03.047. Epub 2016 Mar 31.PMID: 27041491 Review.
Scheen AJ, Marre M, Thivolet C.Diabetes Metab. 2020 Sep;46(4):265-271. doi: 10.1016/j.diabet.2020.05.008. Epub 2020 May 21.PMID: 32447101 Free PMC article. Review.
Cited by
Mild Hyperglycaemia in Hospitalised Children with Moderate COVID-19 Infection.
Vojtková J, Bánovčin P, Ďurdíková A, Nováková E, Jeseňák M.Medicina (Kaunas). 2023 May 14;59(5):944. doi: 10.3390/medicina59050944.PMID: 37241176 Free PMC article.
Schlesinger S, Lang A, Christodoulou N, Linnerz P, Pafili K, Kuss O, Herder C, Neuenschwander M, Barbaresko J, Roden M.Diabetologia. 2023 May 19:1-18. doi: 10.1007/s00125-023-05928-1. Online ahead of print.PMID: 37204441 Free PMC article.
KMEL References
References
-
- WHO Naming the Coronavirus Disease (COVID-19) and the Virus That Causes It. [(accessed on 18 February 2022)];2020 Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technica....
-
- Alqahtani F.Y., Aleanizy F.S., Mohamed R.A.E.H., Alanazi M.S., Mohamed N., Alrasheed M.M., Abanmy N., Alhawassi T. Prevalence of comorbidities in cases of Middle East respiratory syndrome coronavirus: A retrospective study. Epidemiol. Infect. 2019;147:e35. doi: 10.1017/S0950268818002923. - DOI - PMC - PubMed
-
- Yang J.K., Feng Y., Yuan M.Y., Yuan S.Y., Fu H.J., Wu B.Y., Sun G.Z., Yang G.R., Zhang X.L., Wang L., et al. Plasma glucose levels and diabetes are independent predictors for mortality and morbidity in patients with SARS. Diabet. Med. 2006;23:623–628. doi: 10.1111/j.1464-5491.2006.01861.x. - DOI - PubMed
-
- Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z., Xiang J., Wang Y., Song B., Gu X., et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. - DOI - PMC - PubMed
-
- Petrilli C.M., Jones S.A., Yang J., Rajagopalan H., O’Donnell L., Chernyak Y., Tobin K.A., Cerfolio R.J., Francois F., Horwitz L.I. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: Prospective cohort study. BMJ. 2020;369:m1966. doi: 10.1136/bmj.m1966. - DOI - PMC - PubMed
-
- CDC Underlying Medical Conditions Associated with Higher Risk for Severe COVID-19: Information for Healthcare Professionals. [(accessed on 8 March 2022)]; Centers for Disease Control and Prevention. 11 February 2020. Available online: https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/underlyingco....
-
- NHS Who is at High Risk from Coronavirus (COVID-19) [(accessed on 7 March 2022)]; nhs.uk. 1 March 2021. Available online: https://www.nhs.uk/conditions/coronavirus-covid-19/people-at-higher-risk...
-
- Cariou B., Hadjadj S., Wargny M., Pichelin M., Al-Salameh A., Allix I., Amadou C., Arnault G., Baudoux F., Bauduceau B., et al. Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: The CORONADO study. Diabetologia. 2020;63:1500–1515. doi: 10.1007/s00125-020-05180-x. - DOI - PMC - PubMed
-
- Holman N., Knighton P., Kar P., O’Keefe J., Curley M., Weaver A., Barron E., Bakhai C., Khunti K., Wareham N.J., et al. Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: A population-based cohort study. Lancet Diabetes Endocrinol. 2020;8:823–833. doi: 10.1016/S2213-8587(20)30271-0. - DOI - PMC - PubMed
-
- Shi Q., Zhang X., Jiang F., Zhang X., Hu N., Bimu C., Feng J., Yan S., Guan Y., Xu D., et al. Clinical Characteristics and Risk Factors for Mortality of COVID-19 Patients With Diabetes in Wuhan, China: A Two-Center, Retrospective Study. Diabetes Care. 2020;43:1382–1391. doi: 10.2337/dc20-0598. - DOI - PubMed
-
- Wang S., Ma P., Zhang S., Song S., Wang Z., Ma Y., Xu J., Wu F., Duan L., Yin Z., et al. Fasting blood glucose at admission is an independent predictor for 28-day mortality in patients with COVID-19 without previous diagnosis of diabetes: A multi-centre retrospective study. Diabetologia. 2020;63:2102–2111. doi: 10.1007/s00125-020-05209-1. - DOI - PMC - PubMed
-
- Wu J., Huang J., Zhu G., Wang Q., Lv Q., Huang Y., Yu Y., Si X., Yi H., Wang C., et al. Elevation of blood glucose level predicts worse outcomes in hospitalized patients with COVID-19: A retrospective cohort study. BMJ Open Diabetes Res Care. 2020;8:e001476. doi: 10.1136/bmjdrc-2020-001476. - DOI - PMC - PubMed
-
- WHO Novel Coronavirus COVID-19 Therapeutic Trial Synopsis. [(accessed on 2 January 2022)];2020 Available online: https://www.who.int/publications/i/item/covid-19-therapeutic-trial-synopsis.
-
- Al Argan R., Alkhafaji D., Al Elq A., Albaker W., Alqatari S., Alzaki A., Alwaheed A., Al Said A., Bukhari H., Al Warthan S., et al. The Impact of Diabetes Mellitus and Hyperglycemia on the Severity and Outcome of Patients with COVID-19 Disease: A Single-Center Experience. Int. J. Gen. Med. 2021;14:9445–9457. doi: 10.2147/IJGM.S338800. - DOI - PMC - PubMed
-
- Mamtani M., Athavale A.M., Abraham M., Vernik J., Amarah A.R., Ruiz J.P., Joshi A.J., Itteera M., Zhukovski S.D., Madaiah R.P., et al. Association of hyperglycaemia with hospital mortality in nondiabetic COVID-19 patients: A cohort study. Diabetes Metab. 2021;47:101254. doi: 10.1016/j.diabet.2021.101254. - DOI - PMC - PubMed
-
- Marenzi G., Cosentino N., Milazzo V., De Metrio M., Cecere M., Mosca S., Rubino M., Campodonico J., Moltrasio M., Marana I., et al. Prognostic Value of the Acute-to-Chronic Glycemic Ratio at Admission in Acute Myocardial Infarction: A Prospective Study. Diabetes Care. 2018;41:847–853. doi: 10.2337/dc17-1732. - DOI - PubMed
-
- Di Luzio R., Dusi R., Mazzotti A., Petroni M.L., Marchesini G., Bianchi G. Stress Hyperglycemia and Complications Following Traumatic Injuries in Individuals with/without Diabetes: The Case of Orthopedic Surgery. Diabetes Metab. Syndr. Obes. Targets Ther. 2020;13:9–17. doi: 10.2147/DMSO.S225796. - DOI - PMC - PubMed
-
- Yang Y., Kim T.H., Yoon K.H., Chung W.S., Ahn Y., Jeong M.H., Seung K.B., Lee S.H., Chang K. The stress hyperglycemia ratio, an index of relative hyperglycemia, as a predictor of clinical outcomes after percutaneous coronary intervention. Int. J. Cardiol. 2017;241:57–63. doi: 10.1016/j.ijcard.2017.02.065. - DOI - PubMed