Uterine cavity evaluation after uterine preservation surgeries for morbidly adherent placenta
Affiliations
Affiliations
- Department of Obstetrics and Gynaecology, Faculty of Medicine, Ain Shams University, Cairo, Egypt.
- Ahmadi Hospital, Kuwait Oil Company (KOC), Kuwait.
Abstract
Introduction: The morbidly adherent placenta (MAP) is usually associated with maternal morbidity and mortality. The objective of this study was to evaluate the uterine cavity after uterine preservation surgeries for MAP.
Material and methods: The study group comprised women ≥ 28 weeks pregnant with confirmed MAP, with a desire for future fertility, and who agreed to uterine preservation surgery for MAP. The uterine preservation surgeries done for MAP include the following: uterine artery ligation, placental-myometrial en bloc excision, and/or internal iliac artery (IIA) ligation. Participants managed by uterine preservation surgeries for MAP were evaluated 3-6 months after the surgeries using office hysteroscopies to evaluate the uterine cavity after uterine preservation surgeries (primary outcome). The secondary outcome measures the pregnancy outcome after uterine preservation surgery.
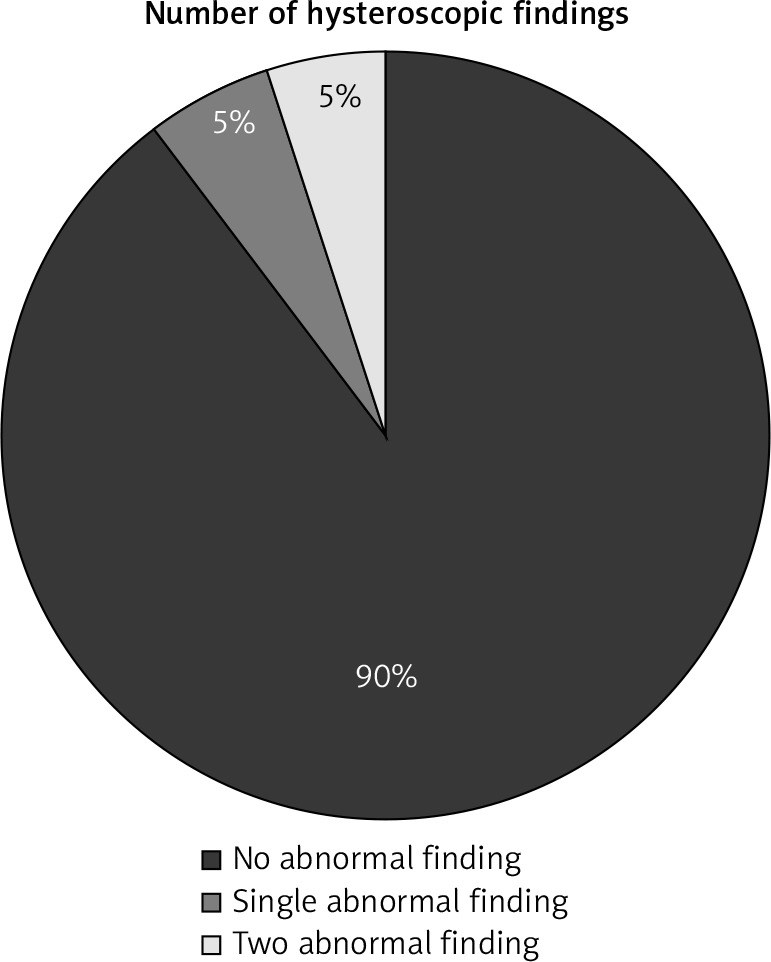
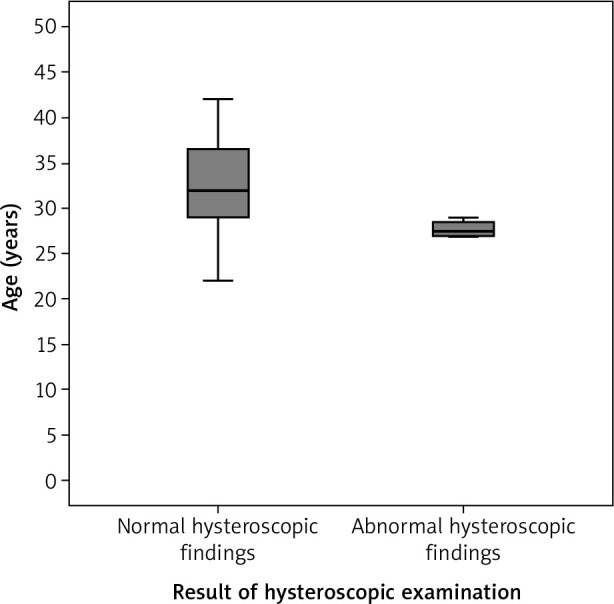
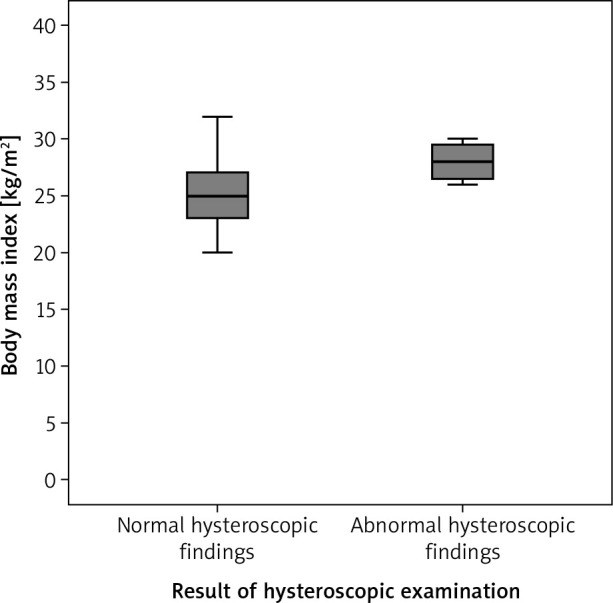
Results: The hysteroscopic examination of the uterine cavity after uterine preservation surgery for MAP showed normal uterine cavity in 36 participants (90%), while it showed abnormal uterine cavity in 4 participants (10%). The abnormal hysteroscopic findings were a single abnormal hysteroscopic finding (endometrial polyp) in 2 participants (5%) and 2 abnormal hysteroscopic findings (incompletely healed scar with unilateral tubal ostial occlusion) in 2 participants (5%). The incidence of pregnancy after uterine preservation surgeries for MAP was 7.5% (3/40).
Conclusions: The uterine preservation surgeries for MAP in this study had no effect on menstrual pattern, uterine cavity, or future fertility. The effect of uterine preservation surgeries for MAP on menstrual pattern, uterine cavity, and future fertility should be evaluated in future larger studies.
Keywords: hysteroscopy; morbidly adherent placenta; surgeries; uterine cavity; uterine preservation.
Conflict of interest statement
The authors report no conflict of interest.
Figures
Similar articles
Hysteroscopy for treating subfertility associated with suspected major uterine cavity abnormalities.
Bosteels J, van Wessel S, Weyers S, Broekmans FJ, D'Hooghe TM, Bongers MY, Mol BWJ.Cochrane Database Syst Rev. 2018 Dec 5;12(12):CD009461. doi: 10.1002/14651858.CD009461.pub4.PMID: 30521679 Free PMC article.
Shmakov RG, Vinitskiy AA, Chuprinin VD, Yarotskaya EL, Sukhikh GT.J Matern Fetal Neonatal Med. 2019 Jun;32(12):2042-2048. doi: 10.1080/14767058.2018.1424821. Epub 2018 Feb 5.PMID: 29402157 Clinical Trial.
El Gelany S, Ibrahim EM, Mohammed M, Abdelraheim AR, Khalifa EM, Abdelhakium AK, Yousef AM, Hassan H, Goma K, Khairy M.BMC Pregnancy Childbirth. 2019 Mar 29;19(1):106. doi: 10.1186/s12884-019-2244-4.PMID: 30922265 Free PMC article.
Hysteroscopy for treating subfertility associated with suspected major uterine cavity abnormalities.
Bosteels J, Kasius J, Weyers S, Broekmans FJ, Mol BW, D'Hooghe TM.Cochrane Database Syst Rev. 2015 Feb 21;(2):CD009461. doi: 10.1002/14651858.CD009461.pub3.PMID: 25701429 Updated. Review.
Hysteroscopy for treating subfertility associated with suspected major uterine cavity abnormalities.
Bosteels J, Kasius J, Weyers S, Broekmans FJ, Mol BW, D'Hooghe TM.Cochrane Database Syst Rev. 2013 Jan 31;(1):CD009461. doi: 10.1002/14651858.CD009461.pub2.PMID: 23440838 Updated. Review.
KMEL References
References
-
- Silver RM, Landon MB, Rouse DJ, et al. . National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Maternal morbidity associated with multiple repeat cesarean deliveries. Obstet Gynecol 2006; 107: 1226-1232. - PubMed
-
- Eller AG, Porter TF, Soisson P, Silver RM. Optimal management strategies for placenta accreta. BJOG 2009; 116: 648-654. - PubMed
-
- Getahun D, Oyelese Y, Salihu HM, Ananth CV. Previous cesarean delivery and risks of placenta previa and placental abruption. Obstet Gynecol 2006; 107: 771-778. - PubMed
-
- Eshkoli T, Weintraub AY, Sergienko R, Sheiner E. Placenta accreta: risk factors, perinatal outcomes and consequences for subsequent births. Am J Obstet Gynecol 2013; 208: e1-7. - PubMed
-
- Hall T, Wax JR, Lucas FL, Cartin A, Jones M, Pinette MG. Prenatal sonographic diagnosis of placenta accreta--impact on maternal and neonatal outcomes. J Clin Ultrasound 2014; 42: 449-455. - PubMed
-
- Warshak CR, Eskander R, Hull AD, et al. . Accuracy of ultrasonography and magnetic resonance imaging in the diagnosis of placenta accreta. Obstet Gynecol 2006; 108: 573-581. - PubMed
-
- D’Antonio F, Bhide A. Ultrasound in placental disorders. Best Pract Res Clin Obstet Gynaecol 2014; 28: 429-442. - PubMed
-
- Moodley J, Ngambu NF, Corr P. Imaging techniques to identify morbidly adherent placenta praevia: a prospective study. J Obstet Gynaecol 2004; 24: 742-744. - PubMed
-
- Fox KA, Shamshirsaz AA, Carusi D, et al. . Conservative management of morbidly adherent placenta: expert review. Am J Obstet Gynecol 2015; 213: 755-760. - PubMed
-
- Gungor T, Simsek A, Ozdemir AO, Pektas M, Danisman N, Mollamahmutoglu L. Surgical treatment of intractable postpartum hemorrhage and changing trends in modern obstetric perspective. Arch Gynecol Obstet 2009; 280: 351-355. - PubMed
-
- Perez-Delboy A, Wright JD. Surgical management of placenta accreta: to leave or remove the placenta? BJOG 2014; 121: 163-169. - PubMed
-
- Abdelazim IA, Elezz AA. Complementary roles of hysteroscopy and saline infusion hysterosonography in uterine cavity assessment before in vitro fertilization. APJR 2012; 1: 13-16.
-
- Comstock CH, Lee W, Vettraino IM, Bronsteen RA. The early sonographic appearance of placenta accreta. J Ultrasound Med 2003; 22: 19-23. - PubMed
-
- Amirabi A, Amjadipour N, Dinparast L. Diagnostic value of doppler ultrasonography in the diagnosis of morbidly adherent placenta. J Obstet Gynecol Cancer Res 2018; 3: 23-28.
-
- Palacios Jaraquemada JM, Pesaresi M, Nassif JC, Hermosid S. Anterior placenta percreta: surgical approach, hemostasis, and uterine repair. Acta Obstet Gynecol Scand 2004; 83: 738-744. - PubMed
-
- Talamonte VH, Lippi UG, Lopes RG, Stabile SA. Hysteroscopic findings in patients with post-menstrual spotting with prior cesarean section. Einstein (Sao Paulo) 2012; 10: 53-56. - PubMed
-
- Bij de Vaate AJ, Brölmann HA, van der Voet LF, van der Slikke JW, Veersema S, Huirne JA. Ultrasound evaluation of the cesarean scar: relation between a niche and postmenstrual spotting. Ultrasound Obstet Gynecol 2011; 37: 93-99. - PubMed
-
- Antila-Långsjö RM, Mäenpää JU, Huhtala HS, Tomás EI, Staff SM. Cesarean scar defect: a prospective study on risk factors. Am J Obstet Gynecol 2018; 219: 458.e1-458.e8. - PubMed
-
- Hayakawa H, Itakura A, Mitsui T, et al. . Methods for myometrium closure and other factors impacting effects on cesarean section scars of the uterine segment detected by the ultrasonography. Acta Obstet Gynecol Scand 2006; 85: 429-434. - PubMed
-
- Bennich G, Rudnicki M, Wilken-Jensen C, Lousen T, Lassen PD, Wøjdemann K. Impact of adding a second layer to a single unlocked closure of a cesarean uterine incision: randomized controlled trial. Ultrasound Obstet Gynecol 2016; 47: 417-422. - PubMed