Detecting spontaneous retroperitoneal hemorrhage using a modified RUSH protocol: a case report
Affiliations
Affiliations
- Critical Care Unit, Ahmadi Hospital, Kuwait Oil Company, PO Box 46468, 64015 Fahahil, Kuwait. Electronic address: zbitar2@hotmail.com.
- Critical Care Unit, Ahamdi Hospital, Kuwait Oil Company, Kuwait. Electronic address: Relshabasy@kockw.com.
- Critical Care Unit, Ahamdi Hospital, Kuwait Oil Company, Kuwait. Electronic address: momohsen@kockw.com.
- Critical Care Unit, Ahmadi Hospital, Kuwait Oil Company, PO Box 46468, 64015 Fahaheel, Kuwait.
- Critical Care Unit, Internal Medicine Dept, Ahmadi Hospital, Kuwait.
- Specialist Internal Medicine, Ahmadi Hospital, KOC, Kuwait. Electronic address: Mgohar@kockw.com.
Abstract
Introduction: Bleeding in the retroperitoneal space is a serious complication. Hypovolemia and shock develop late after losing a large volume of blood. However, point of care ultrasound (POCUS) examinations in adult patients with shock do not include the retroperitoneal space.
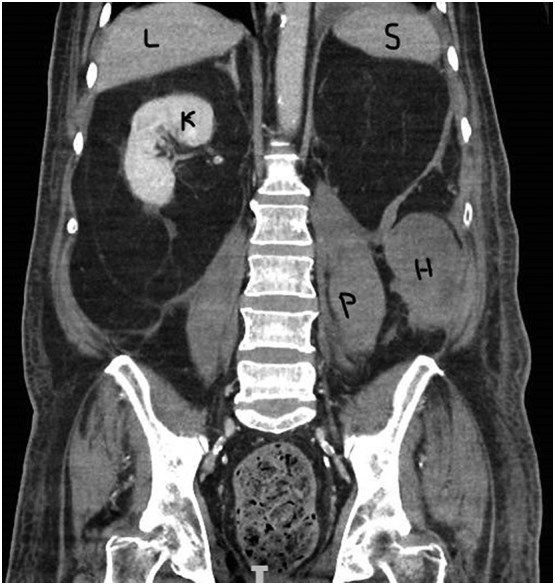
Case presentation: We present the case of a 74-year-old male with ischemic heart disease on dual antiplatelet. He developed vague abdominal pain and hemoglobin drop without overt bleeding source until he developed shock. Modified POCUS examination that included the retroperitoneal space detected the bleeding source and confirmed later by computerized tomography of the abdomen. The case was managed conservatively.
Clinical discussion: The risk factors associated with the formation of spontaneous retroperitoneal hematomas are age above 70 years and dual antiplatelet therapy. The initial integration of point-of-care ultrasound into the assessment of shocked patients leads to an earlier and accurate initial diagnosis with a clear patient care plan. POCUS should include the retroperitoneal space examination in every patient presenting with shock.
Conclusion: In patients with unexplained hemorrhagic shock, a modified POCUS protocol could help by including an examination of the retroperitoneal space in the assessment.
Keywords: Case report; Point of care ultrasound; Retroperitoneal hemorrhage.
Conflict of interest statement
The authors declare no conflicts of interest.
Figures
Similar articles
Antiplatelet Therapy and Spontaneous Retroperitoneal Hematoma: A Case Report and Literature Review.
Ibrahim W, Mohamed A, Sheikh M, Shokr M, Hassan A, Wienberger J, Afonso LC.Am J Case Rep. 2017 Jan 25;18:85-89. doi: 10.12659/ajcr.901622.PMID: 28119516 Free PMC article. Review.
Pain in the hip: Spontaneous retroperitoneal hemorrhage in an elderly patient on apixaban.
Khan A, Mastenbrook J, Bauler L.Am J Emerg Med. 2020 May;38(5):1046.e1-1046.e3. doi: 10.1016/j.ajem.2019.12.049. Epub 2019 Dec 24.PMID: 31932125
Nasr MA, Khallafalla H, Kumar VR, Pathan SA.Qatar Med J. 2019 Aug 1;2019(1):6. doi: 10.5339/qmj.2019.6. eCollection 2019.PMID: 31392172 Free PMC article.
Yang Y, Wang G, Lu H, Liu Y, Ning S, Luo F.BMC Surg. 2020 Nov 30;20(1):304. doi: 10.1186/s12893-020-00953-y.PMID: 33256692 Free PMC article. Review.
Daliakopoulos SI, Bairaktaris A, Papadimitriou D, Pappas P.J Med Case Rep. 2008 May 17;2:162. doi: 10.1186/1752-1947-2-162.PMID: 18485233 Free PMC article.
Cited by
Mavridis C, Lagoudaki E, Georgiadis G, Bouchalakis A, Mamoulakis C.Cureus. 2023 Mar 29;15(3):e36839. doi: 10.7759/cureus.36839. eCollection 2023 Mar.PMID: 37123758 Free PMC article.
KMEL References
References
-
- Sanchez C.E., Helmy T. Percutaneous management of inferior epigastric artery injury after cardiac catheterization. Catheter. Cardiovasc. Interv. 2012;79(4):633–637. - PubMed
-
- Kirkpatrick A.W., Sirois M., Laupland K.B., et al. Hand-held thoracic sonography for detecting post-traumatic pneumothoraces: the extended focused assessment with sonography for trauma (EFAST) J. Trauma. 2004;57(2):288–295. - PubMed
-
- Jones A.E., Tayal V.S., Sullivan D.M., et al. Randomized, controlled trial of immediate versus delayed goal directed ultrasound to identify the cause of nontraumatic hypotension in emergency department patients. Crit. Care Med. 2004;32:1703–1708. - PubMed
-
- Pershad J., Myers S., Plouman C., et al. Bedside limited echocardiography by the emergency physician is accurate during evaluation of the critically ill patient. Pediatrics. 2004;114:e667–e671. - PubMed
-
- Perera P., Mailhot T., Riley D., Mandavia D. The RUSH exam: rapid ultrasound in shock in the evaluation of the critically ill. Emerg. Med. Clin. North Am. 2010;28(1):29–56. - PubMed
-
- Hatjipetrou A., Anyfantakis D., Kastanakis M. Rectus sheath hematoma: a review of the literature. Int. J. Surg. 2015;13:267. - PubMed
-
- Levine M.N., Raskob G., Landefeld S., Kearon C. Hemorrhagic complications of anticoagulant treatment. Chest. 2001;119:108S. - PubMed
-
- Sunga K.L., Bellolio M.F., Gilmore R.M., Cabrera D. Spontaneous retroperitoneal hematoma: etiology, characteristics, management, and outcome. J. Emerg. Med. 2012;43 - PubMed
-
- Sahu K.K., Mishra A.K., Lal A., et al. Clinical spectrum, risk factors, management and outcome of patients with retroperitonealhematoma: a retrospective analysis of 3-year experience. Expert. Rev. Hematol. 2020;13:545. - PubMed
-
- Baekgaard J.S., Eskesen T.G., Lee J.M., Yeh D.D., HMA Kaafarani, Fagenholz P.J., Avery L., Saillant N., King D.R., Velmahos G.C. Spontaneous retroperitoneal and rectus sheath hemorrhage-management, risk factors and outcomes. World J Surg. 2019;43(8):1890–1897. doi: 10.1007/s00268-019-04988-y. - DOI - PubMed
-
- Warren M.H., Bhattacharya B., Maung A.A., Davis K.A. Contemporary management of spontaneous retroperitoneal and rectus sheath hematomas. Am. J. Surg. 2020;219:707. - PubMed