Application of Artificial Intelligence in Combating High Antimicrobial Resistance Rates
Ali A Rabaan 1 2 3, Saad Alhumaid 4, Abbas Al Mutair 5 6 7 8, Mohammed Garout 9, Yem Abulhamayel 10, Muhammad A Halwani 11, Jeehan H Alestad 12 13, Ali Al Bshabshe 14, Tarek Sulaiman 15, Meshal K AlFonaisan 16, Tariq Almusawi 17 18, Hawra Albayat 19, Mohammed Alsaeed 20, Mubarak Alfaresi 21 22, Sultan Alotaibi 23, Yousef N Alhashem 24, Mohamad-Hani Temsah 25, Urooj Ali 26, Naveed Ahmed 27
Affiliations
Affiliations
- 1Molecular Diagnostic Laboratory, Johns Hopkins Aramco Healthcare, Dhahran 31311, Saudi Arabia.
- 2College of Medicine, Alfaisal University, Riyadh 11533, Saudi Arabia.
- 3Department of Public Health and Nutrition, The University of Haripur, Haripur 22610, Pakistan.
- 4Administration of Pharmaceutical Care, Al-Ahsa Health Cluster, Ministry of Health, Al-Ahsa 31982, Saudi Arabia.
- 5Research Center, Almoosa Specialist Hospital, Alhassa, Al-Ahsa 36342, Saudi Arabia.
- 6Almoosa College of Health Sciences, Alhassa, Al-Ahsa 36342, Saudi Arabia.
- 7School of Nursing, Wollongong University, Wollongong, NSW 2522, Australia.
- 8Nursing Department, Prince Sultan Military College of Health Sciences, Dhahran 34313, Saudi Arabia.
- 9Department of Community Medicine and Health Care for Pilgrims, Faculty of Medicine, Umm Al-Qura University, Makkah 21955, Saudi Arabia.
- 10Specialty Internal Medicine Department, Johns Hopkins Aramco Healthcare, Dhahran 34465, Saudi Arabia.
- 11Department of Medical Microbiology, Faculty of Medicine, Al Baha University, Al Baha 4781, Saudi Arabia.
- 12Immunology and Infectious Microbiology Department, University of Glasgow, Glasgow G1 1XQ, UK.
- 13Microbiology Department, Collage of Medicine, Jabriya 46300, Kuwait.
- 14Adult Critical Care Department of Medicine, Division of Adult Critical Care, College of Medicine, King Khalid University, Abha 62561, Saudi Arabia.
- 15Infectious Diseases Section, Medical Specialties Department, King Fahad Medical City, Riyadh 12231, Saudi Arabia.
- 16Basic Medical Sciences, Majmaah University, Majmaah 11952, Saudi Arabia.
- 17Infectious Disease and Critical Care Medicine Department, Dr. Sulaiman Alhabib Medical Group, Alkhobar 34423, Saudi Arabia.
- 18Department of Medicine, Royal College of Surgeons in Ireland-Medical University of Bahrain, Manama 15503, Bahrain.
- 19Infectious Disease Department, King Saud Medical City, Riyadh 7790, Saudi Arabia.
- 20Infectious Disease Division, Department of Medicine, Prince Sultan Military Medical City, Riyadh 11159, Saudi Arabia.
- 21Department of Pathology and Laboratory Medicine, Sheikh Khalifa General Hospital, Umm Al Quwain 499, United Arab Emirates.
- 22Department of Pathology, College of Medicine, Mohammed Bin Rashid University of Medicine and Health Sciences, Dubai 505055, United Arab Emirates.
- 23Molecular Microbiology Department, King Fahad Medical City, Riyadh 11525, Saudi Arabia.
- 24Department of Clinical Laboratory Sciences, Mohammed AlMana College of Health Sciences, Dammam 34222, Saudi Arabia.
- 25Pediatric Department, College of Medicine, King Saud University, Riyadh 11451, Saudi Arabia.
- 26Department of Biotechnology, Faculty of Life Sciences, University of Central Punjab, Lahore 54000, Pakistan.
- 27Department of Medical Microbiology and Parasitology, School of Medical Sciences, Universiti Sains Malaysia, Kubang Kerian, Kota Bharu 16150, Kelantan, Malaysia.
Abstract
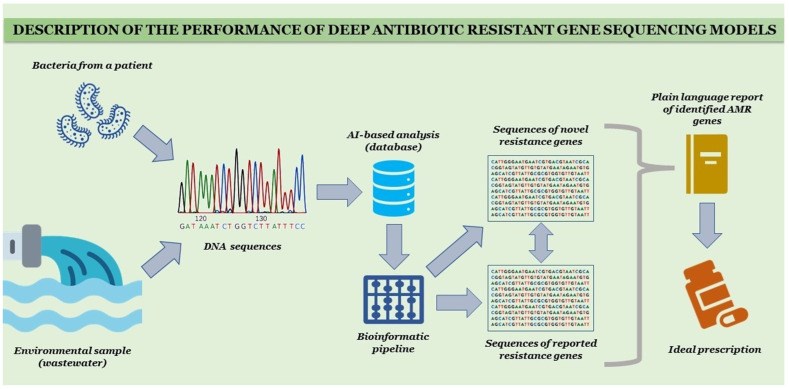
Artificial intelligence (AI) is a branch of science and engineering that focuses on the computational understanding of intelligent behavior. Many human professions, including clinical diagnosis and prognosis, are greatly useful from AI. Antimicrobial resistance (AMR) is among the most critical challenges facing Pakistan and the rest of the world. The rising incidence of AMR has become a significant issue, and authorities must take measures to combat the overuse and incorrect use of antibiotics in order to combat rising resistance rates. The widespread use of antibiotics in clinical practice has not only resulted in drug resistance but has also increased the threat of super-resistant bacteria emergence. As AMR rises, clinicians find it more difficult to treat many bacterial infections in a timely manner, and therapy becomes prohibitively costly for patients. To combat the rise in AMR rates, it is critical to implement an institutional antibiotic stewardship program that monitors correct antibiotic use, controls antibiotics, and generates antibiograms. Furthermore, these types of tools may aid in the treatment of patients in the event of a medical emergency in which a physician is unable to wait for bacterial culture results. AI's applications in healthcare might be unlimited, reducing the time it takes to discover new antimicrobial drugs, improving diagnostic and treatment accuracy, and lowering expenses at the same time. The majority of suggested AI solutions for AMR are meant to supplement rather than replace a doctor's prescription or opinion, but rather to serve as a valuable tool for making their work easier. When it comes to infectious diseases, AI has the potential to be a game-changer in the battle against antibiotic resistance. Finally, when selecting antibiotic therapy for infections, data from local antibiotic stewardship programs are critical to ensuring that these bacteria are treated quickly and effectively. Furthermore, organizations such as the World Health Organization (WHO) have underlined the necessity of selecting the appropriate antibiotic and treating for the shortest time feasible to minimize the spread of resistant and invasive resistant bacterial strains.
Keywords: AMR; advances; antibiotic stewardship; better diagnosis; diagnostic microbiology; global platform.
Conflict of interest statement
The authors declare no conflict of interest.
Figures
Similar articles
Using Machine Learning to Predict Antimicrobial Resistance-A Literature Review.
Sakagianni A, Koufopoulou C, Feretzakis G, Kalles D, Verykios VS, Myrianthefs P, Fildisis G.Antibiotics (Basel). 2023 Feb 24;12(3):452. doi: 10.3390/antibiotics12030452.PMID: 36978319 Free PMC article. Review.
Role of Artificial Intelligence in Fighting Antimicrobial Resistance in Pediatrics.
Fanelli U, Pappalardo M, Chinè V, Gismondi P, Neglia C, Argentiero A, Calderaro A, Prati A, Esposito S.Antibiotics (Basel). 2020 Nov 1;9(11):767. doi: 10.3390/antibiotics9110767.PMID: 33139605 Free PMC article. Review.
Spera AM, Esposito S, Pagliano P.Infez Med. 2019 Dec 1;27(4):357-364.PMID: 31846984 Review.
[No authors listed]Washington (DC): American Society for Microbiology; 2009.PMID: 32644325 Free Books & Documents. Review.
Gulumbe BH, Haruna UA, Almazan J, Ibrahim IH, Faggo AA, Bazata AY.Biol Proced Online. 2022 Nov 23;24(1):19. doi: 10.1186/s12575-022-00182-y.PMID: 36424530 Free PMC article. Review.
Cited by
Ali T, Ahmed S, Aslam M.Antibiotics (Basel). 2023 Mar 6;12(3):523. doi: 10.3390/antibiotics12030523.PMID: 36978390 Free PMC article. Review.
Girija ASS, Gunasekaran S, Habib S, Aljeldah M, Al Shammari BR, Alshehri AA, Alwashmi ASS, Turkistani SA, Alawfi A, Alshengeti A, Garout M, Alwarthan S, Alsubki RA, Moustafa NM, Rabaan AA.Medicina (Kaunas). 2023 Feb 11;59(2):343. doi: 10.3390/medicina59020343.PMID: 36837545 Free PMC article.
Yadalam PK, Anegundi RV, Munawar S, Ramadoss R, Rengaraj S, Ramesh S, Aljeldah M, Shammari BRA, Alshehri AA, Alwashmi ASS, Turkistani SA, Alawfi A, Alshengeti A, Garout M, Sabour AA, Alshiekheid MA, Aljebaly FS, Rabaan AA.Medicina (Kaunas). 2023 Feb 6;59(2):302. doi: 10.3390/medicina59020302.PMID: 36837503 Free PMC article.
Sohail M, Muzzammil M, Ahmad M, Rehman S, Garout M, Khojah TM, Al-Eisa KM, Breagesh SA, Hamdan RMA, Alibrahim HI, Alsoliabi ZA, Rabaan AA, Ahmed N.Antibiotics (Basel). 2023 Jan 12;12(1):157. doi: 10.3390/antibiotics12010157.PMID: 36671358 Free PMC article.
Mustafai MM, Hafeez M, Munawar S, Basha S, Rabaan AA, Halwani MA, Alawfi A, Alshengeti A, Najim MA, Alwarthan S, AlFonaisan MK, Almuthree SA, Garout M, Ahmed N.Antibiotics (Basel). 2023 Jan 11;12(1):148. doi: 10.3390/antibiotics12010148.PMID: 36671350 Free PMC article.
KMEL References
References
-
- Susmita R.C., Zubayed A., Krishna R., Abdullah A.N., Rashid M.H., Kamol C.M. Emerging threats of antibiotic resistance in Salmonella typhi and Salmonella paratyphi A among enteric fever cases of Dhaka, Bangladesh. Afr. J. Bacteriol. Res. 2022;14:8–15.
-
- Gemert T.V. Bachelor’s Thesis. Utrecht University; Utrecht, The Netherlands: 2017. On the Influence of Dataset Characteristics on Classifier Performance.
-
- Ahmed N., Zeshan B., Naveed M., Afzal M., Mohamed M. Antibiotic resistance profile in relation to virulence genes fimH, hlyA and usp of uropathogenic E. coli isolates in Lahore, Pakistan. Trop. Biomed. 2019;36:559–568. - PubMed
-
- Lv J., Deng S., Zhang L. A review of artificial intelligence applications for antimicrobial resistance. Biosaf. Health. 2021;3:22–31. doi: 10.1016/j.bsheal.2020.08.003. - DOI
-
- Raisch S., Krakowski S. Artificial intelligence and management: The automation–augmentation paradox. Acad. Manag. Rev. 2021;46:192–210. doi: 10.5465/amr.2018.0072. - DOI
-
- Song L., Gildea D., Zhang Y., Wang Z., Su J. Semantic neural machine translation using AMR. Trans. Assoc. Comput. Linguist. 2019;7:19–31. doi: 10.1162/tacl_a_00252. - DOI
-
- Williams M.A., Wyner S.N. Antimicrobial Resistance: Facing the Rise of a Global Threat. American Public Health Association; Washington, DC, USA: 2019.
-
- Fasih N., Zafar A., Khan E., Jabeen K., Hasan R. Clonal dissemination of vanA positive Enterococcus species in tertiary care hospitals in Karachi, Pakistan. J. Pak. Med. Assoc. 2010;60:805. - PubMed
-
- Miller J.R., Dunham S., Mochalkin I., Banotai C., Bowman M., Buist S., Dunkle B., Hanna D., Harwood H.J., Huband M.D. A class of selective antibacterials derived from a protein kinase inhibitor pharmacophore. Proc. Natl. Acad. Sci. USA. 2009;106:1737–1742. doi: 10.1073/pnas.0811275106. - DOI - PMC - PubMed
-
- Cánovas-Segura B., Campos M., Morales A., Juarez J.M., Palacios F. Development of a clinical decision support system for antibiotic management in a hospital environment. Prog. Artif. Intell. 2016;5:181–197. doi: 10.1007/s13748-016-0089-x. - DOI
-
- Zafar A., Hasan R., Nizami S.Q., von Seidlein L., Soofi S., Ahsan T., Chandio S., Habib A., Bhutto N., Siddiqui F.J. Frequency of isolation of various subtypes and antimicrobial resistance of Shigella from urban slums of Karachi, Pakistan. Int. J. Infect. Dis. 2009;13:668–672. doi: 10.1016/j.ijid.2008.10.005. - DOI - PubMed
-
- Parveen S., Saqib S., Ahmed A., Shahzad A., Ahmed N. Prevalence of MRSA colonization among healthcare-workers and effectiveness of decolonization regimen in ICU of a Tertiary care Hospital, Lahore, Pakistan. Adv. Life Sci. 2020;8:38–41.
-
- Zeshan B., Karobari M.I., Afzal N., Siddiq A., Basha S., Basheer S.N., Peeran S.W., Mustafa M., Daud N.H.A., Ahmed N. The usage of antibiotics by COVID-19 patients with comorbidities: The risk of increased antimicrobial resistance. Antibiotics. 2021;11:35. doi: 10.3390/antibiotics11010035. - DOI - PMC - PubMed
-
- Pakistan Antimicrobial Resistance Network (PARN) [(accessed on 20 May 2022)]. Available online: https://parn.org.pk/antimicrobial-data/
-
- Ahmed Z., Bhinder K.K., Tariq A., Tahir M.J., Mehmood Q., Tabassum M.S., Malik M., Aslam S., Asghar M.S., Yousaf Z. Knowledge, attitude, and practice of artificial intelligence among doctors and medical students in Pakistan: A cross-sectional online survey. Ann. Med. Surg. 2022;76:103493. doi: 10.1016/j.amsu.2022.103493. - DOI - PMC - PubMed
-
- Rasheed M.A., Chand P., Ahmed S., Sharif H., Hoodbhoy Z., Siddiqui A., Hasan B.S. Use of artificial intelligence on Electroencephalogram (EEG) waveforms to predict failure in early school grades in children from a rural cohort in Pakistan. PLoS ONE. 2021;16:e0246236. doi: 10.1371/journal.pone.0246236. - DOI - PMC - PubMed
-
- Kazi A.M., Qazi S.A., Khawaja S., Ahsan N., Ahmed R.M., Sameen F., Mughal M.A.K., Saqib M., Ali S., Kaleemuddin H. An artificial intelligence–based, personalized smartphone app to improve childhood immunization coverage and timelines among children in Pakistan: Protocol for a randomized controlled trial. JMIR Res. Protoc. 2020;9:e22996. doi: 10.2196/22996. - DOI - PMC - PubMed
-
- Dahri A.S., Al-Athwari A., Hussain A. Usability evaluation of mobile health application from AI perspective in rural areas of Pakistan. [(accessed on 22 May 2022)];Int. Assoc. Online Eng. 2019 Available online: https://www.learntechlib.org/p/216620/
-
- Khan A.U., Melzer F., Hendam A., Sayour A.E., Khan I., Elschner M.C., Younus M., Ehtisham-ul-Haque S., Waheed U., Farooq M. Seroprevalence and Molecular Identification of Brucella spp. in Bovines in Pakistan—Investigating Association with Risk Factors Using Machine Learning. Front. Vet. Sci. 2020;7:980. doi: 10.3389/fvets.2020.594498. - DOI - PMC - PubMed
-
- Elyan E., Hussain A., Sheikh A., Elmanama A.A., Vuttpittayamongkol P., Hijazi K. Antimicrobial Resistance and Machine Learning: Challenges and Opportunities. IEEE Access. 2022;10:31561–31577. doi: 10.1109/ACCESS.2022.3160213. - DOI
-
- Steinkey R., Moat J., Gannon V., Zovoilis A., Laing C. Application of artificial intelligence to the in silico assessment of antimicrobial resistance and risks to human and animal health presented by priority enteric bacterial pathogens. Can. Commun. Dis. Rep. 2020;46:180–185. doi: 10.14745/ccdr.v46i06a05. - DOI - PMC - PubMed
-
- Wang T., Wan X., Yao S. Better AMR-to-text generation with graph structure reconstruction; Proceedings of the Twenty-Ninth International Conference on International Joint Conferences on Artificial Intelligence; Yokohama, Japan. 7–15 January 2021; pp. 3919–3925.
-
- Van Steenkiste T., Ruyssinck J., De Baets L., Decruyenaere J., De Turck F., Ongenae F., Dhaene T. Accurate prediction of blood culture outcome in the intensive care unit using long short-term memory neural networks. Artif. Intell. Med. 2019;97:38–43. doi: 10.1016/j.artmed.2018.10.008. - DOI - PubMed
-
- Smith K.P., Wang H., Durant T.J.S., Mathison B.A., Sharp S.E., Kirby J.E., Long S.W., Rhoads D.D. Applications of Artificial Intelligence in Clinical Microbiology Diagnostic Testing. Clin. Microbiol. Newsl. 2020;42:61–70. doi: 10.1016/j.clinmicnews.2020.03.006. - DOI
-
- Cartelle Gestal M., Dedloff M.R., Torres-Sangiao E. Computational health engineering applied to model infectious diseases and antimicrobial resistance spread. Appl. Sci. 2019;9:2486. doi: 10.3390/app9122486. - DOI
-
- Khaledi A., Weimann A., Schniederjans M., Asgari E., Kuo T.H., Oliver A., Cabot G., Kola A., Gastmeier P., Hogardt M. Predicting antimicrobial resistance in Pseudomonas aeruginosa with machine learning-enabled molecular diagnostics. EMBO Mol. Med. 2020;12:e10264. doi: 10.15252/emmm.201910264. - DOI - PMC - PubMed
-
- Kayid A. The Role of Artificial Intelligence in Future Technology. Academic Press; Cambridge, MA, USA: 2020. - DOI
-
- VanOeffelen M., Nguyen M., Aytan-Aktug D., Brettin T., Dietrich E.M., Kenyon R.W., Machi D., Mao C., Olson R., Pusch G.D. A genomic data resource for predicting antimicrobial resistance from laboratory-derived antimicrobial susceptibility phenotypes. Brief. Bioinform. 2021;22:bbab313. doi: 10.1093/bib/bbab313. - DOI - PMC - PubMed
-
- Rodríguez-González A., Zanin M., Menasalvas-Ruiz E. Public health and epidemiology informatics: Can artificial intelligence help future global challenges? An overview of antimicrobial resistance and impact of climate change in disease epidemiology. Yearb. Med. Inform. 2019;28:224–231. doi: 10.1055/s-0039-1677910. - DOI - PMC - PubMed
-
- Santerre J.W., Davis J.J., Xia F., Stevens R. Machine learning for antimicrobial resistance. arXiv. 20161607.01224
-
- Feretzakis G., Sakagianni A., Loupelis E., Kalles D., Skarmoutsou N., Martsoukou M., Christopoulos C., Lada M., Petropoulou S., Velentza A. Machine Learning for Antibiotic Resistance Prediction: A Prototype Using Off-the-Shelf Techniques and Entry-Level Data to Guide Empiric Antimicrobial Therapy. Healthc. Inform. Res. 2021;27:214–221. doi: 10.4258/hir.2021.27.3.214. - DOI - PMC - PubMed
-
- Ahmed N., Khalid H., Mushtaq M., Basha S., Rabaan A.A., Garout M., Halwani M.A., Al Mutair A., Alhumaid S., Al Alawi Z., et al. The Molecular Characterization of Virulence Determinants and Antibiotic Resistance Patterns in Human Bacterial Uropathogens. Antibiotics. 2022;11:516. doi: 10.3390/antibiotics11040516. - DOI - PMC - PubMed
-
- Zahra N., Zeshan B., Qadri M.M.A., Ishaq M., Afzal M., Ahmed N. Phenotypic and Genotypic Evaluation of Antibiotic Resistance of Acinetobacter baumannii Bacteria Isolated from Surgical Intensive Care Unit Patients in Pakistan. Jundishapur J. Microbiol. 2021;14:104922. doi: 10.5812/jjm.113008. - DOI
-
- Saleem Z., Godman B., Azhar F., Kalungia A.C., Fadare J., Opanga S., Markovic-Pekovic V., Hoxha I., Saeed A., Al-Gethamy M. Progress on the national action plan of Pakistan on antimicrobial resistance (AMR): A narrative review and the implications. Expert Rev. Anti-Infect. Ther. 2022;20:71–93. doi: 10.1080/14787210.2021.1935238. - DOI - PubMed
-
- Oluwafemi R., Olawale I., Alagbe J. Recent trends in the utilization of medicinal plants as growth promoters in poultry nutrition—A review. Res. Agric. Vet. Sci. 2020;4:5–11.