An update on the management of non-variceal upper gastrointestinal bleeding
Affiliations
Affiliations
- 1Division of Gastroenterology, Department of medicine, Faculty of Medicine, Kuwait University, Kuwait.
- 2Division of Gastroenterology, McGill University Health Center, McGill University, Montreal, Canada.
Abstract
Upper gastrointestinal bleeding (UGIB) continues to be a common gastrointestinal emergency that carries significant morbidity and mortality. The epidemiology of UGIB has been changing over the last few decades with an overall decrease in peptic ulcer disease and increase in the prevalence of other etiologies including vascular lesions and malignancy. Appropriate risk assessment and patient stratification are crucial to ensuring that optimal care is delivered to patients and some risk assessment tools have shown excellent ability to define a low-risk group who can be managed as outpatients safely. Regardless of the etiology of UGIB, resuscitative interventions by primary care providers remain the most important initial measures to improve the outcome for patients including hemodynamic stabilization, an appropriate blood transfusion strategy, with or without acid-lowering agents, while also providing subsequent urgent endoscopic assessment and intervention. In addition, with increasing use of antithrombotic agents in clinical practice and its associated risk of bleeding, the management of such agents in the acute setting has become a real challenge to all physicians. In this article, we provide an up-to-date, evidence-based, practical review of recent changes and advances in UGIB with a focus on non-variceal etiologies.
Keywords: UGIB; antithrombotic; endoscopic hemostasis; peptic ulcer; risk assessment.
Conflict of interest statement
None declared.
Figures
Similar articles
Acute upper gastrointestinal bleeding (UGIB) - initial evaluation and management.
Khamaysi I, Gralnek IM.Best Pract Res Clin Gastroenterol. 2013 Oct;27(5):633-8. doi: 10.1016/j.bpg.2013.09.002. Epub 2013 Sep 25.PMID: 24160923 Review.
Wang J, Cui Y, Wang J, Chen B, He Y, Chen M.Zhonghua Wei Chang Wai Ke Za Zhi. 2017 Apr 25;20(4):425-431.PMID: 28440524 Chinese.
Etiology and adverse outcome predictors of upper gastrointestinal bleeding in 589 patients in Nepal.
Shrestha UK, Sapkota S.Dig Dis Sci. 2014 Apr;59(4):814-22. doi: 10.1007/s10620-013-2946-9. Epub 2013 Nov 27.PMID: 24282053
Prosenz J, Stättermayer MS, Riedl F, Maieron A.Scand J Gastroenterol. 2023 Feb 28:1-7. doi: 10.1080/00365521.2023.2183734. Online ahead of print.PMID: 36855301
Mullady DK, Wang AY, Waschke KA.Gastroenterology. 2020 Sep;159(3):1120-1128. doi: 10.1053/j.gastro.2020.05.095. Epub 2020 Jun 20.PMID: 32574620 Review.
KMEL References
References
-
- Abougergi MS, Travis AC, Saltzman JR.. The in-hospital mortality rate for upper GI hemorrhage has decreased over 2 decades in the United States: a nationwide analysis. Gastrointest Endosc 2015;81:882–8.e1. - PubMed
-
- Patel SD, Desai R, Patel U. et al. Thirty-day readmissions after upper and lower gastrointestinal hemorrhage: a national perspective in the United States. J Clin Gastroenterol 2019;53:582–90. - PubMed
-
- Wuerth BA, Rockey DC.. Changing epidemiology of upper gastrointestinal hemorrhage in the last decade: a nationwide analysis. Dig Dis Sci 2018;63:1286–93. - PubMed
-
- Gupta A, Agarwal R, Ananthakrishnan AN.. “Weekend effect” in patients with upper gastrointestinal hemorrhage: a systematic review and meta-analysis. Am J Gastroenterol 2018;113:13–21. - PubMed
-
- van Leerdam ME. Epidemiology of acute upper gastrointestinal bleeding. Best Pract Res Clin Gastroenterol 2008;22:209–24. - PubMed
-
- Rockall TA, Logan RF, Devlin HB. et al. Variation in outcome after acute upper gastrointestinal haemorrhage: the National Audit of Acute Upper Gastrointestinal Haemorrhage. Lancet 1995;346:346–50. - PubMed
-
- Longstreth GF. Epidemiology of hospitalization for acute upper gastrointestinal hemorrhage: a population-based study. Am J Gastroenterol 1995;90:206–10. - PubMed
-
- Boonpongmanee S, Fleischer DE, Pezzullo JC. et al. The frequency of peptic ulcer as a cause of upper-GI bleeding is exaggerated. Gastrointest Endosc 2004;59:788–94. - PubMed
-
- Enestvedt BK, Gralnek IM, Mattek N. et al. An evaluation of endoscopic indications and findings related to nonvariceal upper-GI hemorrhage in a large multicenter consortium. Gastrointest Endosc 2008;67:422–9. - PubMed
-
- Loperfido S, Baldo V, Piovesana E. et al. Changing trends in acute upper-GI bleeding: a population-based study. Gastrointest Endosc 2009;70:212–24. - PubMed
-
- Sonnenberg A, Turner KO, Genta RM.. Low prevalence of helicobacter pylori-positive peptic ulcers in private outpatient endoscopy centers in the United States. Am J Gastroenterol 2020;115:244–50. - PubMed
-
- Yuan C, Adeloye D, Luk TT. et al. The global prevalence of and factors associated with Helicobacter pylori infection in children: a systematic review and meta-analysis. Lancet Child Adolescent Health 2022;6:185–94. - PubMed
-
- Forrest JA, Finlayson ND, Shearman DJ.. Endoscopy in gastrointestinal bleeding. Lancet 1974;2:394–7. - PubMed
-
- Balderas V, Bhore R, Lara LF. et al. The hematocrit level in upper gastrointestinal hemorrhage: safety of endoscopy and outcomes. Am J Med 2011;124:970–6. - PubMed
-
- Costa ND, Cadiot G, Merle C. et al. Bleeding reflux esophagitis: a prospective 1-year study in a university hospital. Am J Gastroenterol 2001;96:47–51. - PubMed
-
- Rath HC, Timmer A, Kunkel C. et al. Comparison of interobserver agreement for different scoring systems for reflux esophagitis: impact of level of experience. Gastrointest Endosc 2004;60:44–9. - PubMed
-
- Guntipalli P, Chason R, Elliott A. et al. Upper gastrointestinal bleeding caused by severe esophagitis: a unique clinical syndrome. Dig Dis Sci 2014;59:2997–3003. - PubMed
-
- Park CH, Min SW, Sohn YH. et al. A prospective, randomized trial of endoscopic band ligation vs. epinephrine injection for actively bleeding Mallory-Weiss syndrome. Gastrointest Endosc 2004;60:22–7. - PubMed
-
- Llach J, Elizalde JI, Guevara MC. et al. Endoscopic injection therapy in bleeding Mallory-Weiss syndrome: a randomized controlled trial. Gastrointest Endosc 2001;54:679–81. - PubMed
-
- Laine L, Barkun AN, Saltzman JR. et al. ACG Clinical Guideline: upper gastrointestinal and ulcer bleeding. Am J Gastroenterol 2021;116:899–917. - PubMed
-
- Lecleire S, Antonietti M, Iwanicki-Caron I. et al. Endoscopic band ligation could decrease recurrent bleeding in Mallory-Weiss syndrome as compared to haemostasis by hemoclips plus epinephrine. Aliment Pharmacol Ther 2009;30:399–405. - PubMed
-
- Baracat FI, de Moura DTH, Brunaldi VO. et al. Randomized controlled trial of hemostatic powder versus endoscopic clipping for non-variceal upper gastrointestinal bleeding. Surg Endosc 2020;34:317–24. - PubMed
-
- Chahal D, Lee JGH, Ali-Mohamad N. et al. High rate of re-bleeding after application of Hemospray for upper and lower gastrointestinal bleeds. Dig Liver Dis 2020;52:768–72. - PubMed
-
- Yano T, Yamamoto H, Sunada K. et al. Endoscopic classification of vascular lesions of the small intestine (with videos). Gastrointest Endosc 2008;67:169–72. - PubMed
-
- Clouse RE, Costigan DJ, Mills BA. et al. Angiodysplasia as a cause of upper gastrointestinal bleeding. Arch Intern Med 1985;145:458–61. - PubMed
-
- Marwick T, Kerlin P.. Angiodysplasia of the upper gastrointestinal tract: clinical spectrum in 41 cases. J Clin Gastroenterol 1986;8:404–7. - PubMed
-
- Gunnlaugsson O. Angiodysplasia of the stomach and duodenum. Gastrointest Endosc 1985;31:251–4. - PubMed
-
- Chalasani N, Cotsonis G, Wilcox CM.. Upper gastrointestinal bleeding in patients with chronic renal failure: role of vascular ectasia. Am J Gastroenterol 1996;91:2329–32. - PubMed
-
- Alhumood SA, Devine DV, Lawson L. et al. Idiopathic immune-mediated acquired von Willebrand's disease in a patient with angiodysplasia: demonstration of an unusual inhibitor causing a functional defect and rapid clearance of von Willebrand factor. Am J Hematol 1999;60:151–7. - PubMed
-
- Pate GE, Mulligan A.. An epidemiological study of Heyde's syndrome: an association between aortic stenosis and gastrointestinal bleeding. J Heart Valve Dis 2004;13:713–6. - PubMed
-
- Singh G, Albeldawi M, Kalra SS. et al. Features of patients with gastrointestinal bleeding after implantation of ventricular assist devices. Clin Gastroenterol Hepatol 2015;13:107–14.e1. - PubMed
-
- Demirozu ZT, Radovancevic R, Hochman LF. et al. Arteriovenous malformation and gastrointestinal bleeding in patients with the HeartMate II left ventricular assist device. J Heart Lung Transplant 2011;30:849–53. - PubMed
-
- Selinger CP, Ang YS.. Gastric antral vascular ectasia (GAVE): an update on clinical presentation, pathophysiology and treatment. Digestion 2008;77:131–7. - PubMed
-
- Dulai GS, Jensen DM, Kovacs TO. et al. Endoscopic treatment outcomes in watermelon stomach patients with and without portal hypertension. Endoscopy 2004;36:68–72. - PubMed
-
- McCarty TR, Rustagi T.. Comparative effectiveness and safety of radiofrequency ablation versus argon plasma coagulation for treatment of gastric antral vascular ectasia: a systematic review and meta-analysis. J Clin Gastroenterol 2019;53:599–606. - PubMed
-
- Park CH, Joo YE, Kim HS. et al. A prospective, randomized trial of endoscopic band ligation versus endoscopic hemoclip placement for bleeding gastric Dieulafoy's lesions. Endoscopy 2004;36:677–81. - PubMed
-
- Ahn DW, Lee SH, Park YS. et al. Hemostatic efficacy and clinical outcome of endoscopic treatment of Dieulafoy's lesions: comparison of endoscopic hemoclip placement and endoscopic band ligation. Gastrointest Endosc 2012;75:32–8. - PubMed
-
- Savides TJ, Jensen DM, Cohen J. et al. Severe upper gastrointestinal tumor bleeding: endoscopic findings, treatment, and outcome. Endoscopy 1996;28:244–8. - PubMed
-
- Alali A, Moosavi S, Martel M. et al. Topical hemostatic agents in the management of upper gastrointestinal bleeding: a meta-analysis. Endosc Int Open 2022. 10.1055/a-1984-6895. - DOI
-
- Oakland K. Risk stratification in upper and upper and lower GI bleeding: which scores should we use? Best Pract Res Clin Gastroenterol 2019;42–43:101613. - PubMed
-
- Gralnek IM, Stanley AJ, Morris AJ. et al. Endoscopic diagnosis and management of nonvariceal upper gastrointestinal hemorrhage (NVUGIH): European Society of Gastrointestinal Endoscopy (ESGE) Guideline—Update 2021. Endoscopy 2021;53:300–32. - PubMed
-
- Cheng HC, Wu CT, Chang WL. et al. Double oral esomeprazole after a 3-day intravenous esomeprazole infusion reduces recurrent peptic ulcer bleeding in high-risk patients: a randomised controlled study. Gut 2014;63:1864–72. - PubMed
-
- Bryant RV, Kuo P, Williamson K. et al. Performance of the Glasgow-Blatchford score in predicting clinical outcomes and intervention in hospitalized patients with upper GI bleeding. Gastrointest Endosc 2013;78:576–83. - PubMed
-
- Blatchford O, Murray WR, Blatchford M.. A risk score to predict need for treatment for upper-gastrointestinal haemorrhage. Lancet 2000;356:1318–21. - PubMed
-
- Gu L, Xu F, Yuan J.. Comparison of AIMS65, Glasgow-Blatchford and Rockall scoring approaches in predicting the risk of in-hospital death among emergency hospitalized patients with upper gastrointestinal bleeding: a retrospective observational study in Nanjing, China. BMC Gastroenterol 2018;18:98. - PMC - PubMed
-
- Oakland K, Kahan BC, Guizzetti L. et al. Development, validation, and comparative assessment of an international scoring system to determine risk of upper gastrointestinal bleeding. Clin Gastroenterol Hepatol 2019;17:1121–9.e2. - PubMed
-
- Saltzman JR, Tabak YP, Hyett BH. et al. A simple risk score accurately predicts in-hospital mortality, length of stay, and cost in acute upper GI bleeding. Gastrointest Endosc 2011;74:1215–24. - PubMed
-
- Abougergi MS, Charpentier JP, Bethea E. et al. A prospective, multicenter study of the AIMS65 score compared with the Glasgow-Blatchford score in predicting upper gastrointestinal hemorrhage outcomes. J Clin Gastroenterol 2016;50:464–9. - PubMed
-
- Laursen SB, Oakland K, Laine L. et al. ABC score: a new risk score that accurately predicts mortality in acute upper and lower gastrointestinal bleeding: an international multicentre study. Gut 2021;70:707–16. - PubMed
-
- Kherad O, Restellini S, Almadi M. et al. Comparative evaluation of the ABC score to other risk stratification scales in managing high-risk patients presenting with acute upper gastrointestinal bleeding. J Clin Gastroenterol 2022. https://doi.org/10.1097/MCG.0000000000001720. - DOI
-
- Mules TC, Stedman C, Ding S. et al. Comparison of risk scoring systems in hospitalised patients who develop upper gastrointestinal bleeding. GastroHep 2021;3:5–11.
-
- Ramaekers R, Mukarram M, Smith CA. et al. The predictive value of preendoscopic risk scores to predict adverse outcomes in emergency department patients with upper gastrointestinal bleeding: a systematic review. Acad Emerg Med 2016;23:1218–27. - PubMed
-
- Robertson M, Majumdar A, Boyapati R. et al. Risk stratification in acute upper GI bleeding: comparison of the AIMS65 score with the Glasgow-Blatchford and Rockall scoring systems. Gastrointest Endosc 2016;83:1151–60. - PubMed
-
- Martínez-Cara JG, Jiménez-Rosales R, Úbeda-Muñoz M. et al. Comparison of AIMS65, Glasgow-Blatchford score, and Rockall score in a European series of patients with upper gastrointestinal bleeding: performance when predicting in-hospital and delayed mortality. United European Gastroenterol J 2016;4:371–9. - PMC - PubMed
-
- Thanapirom K, Ridtitid W, Rerknimitr R. et al. Prospective comparison of three risk scoring systems in non-variceal and variceal upper gastrointestinal bleeding. J Gastroenterol Hepatol 2016;31:761–7. - PubMed
-
- Laursen SB, Hansen JM, Schaffalitzky de Muckadell OB.. The Glasgow Blatchford score is the most accurate assessment of patients with upper gastrointestinal hemorrhage. Clin Gastroenterol Hepatol 2012;10:1130–5.e1. - PubMed
-
- Odutayo A, Desborough MJ, Trivella M. et al. Restrictive versus liberal blood transfusion for gastrointestinal bleeding: a systematic review and meta-analysis of randomised controlled trials. Lancet Gastroenterol Hepatol 2017;2:354–60. - PubMed
-
- Barkun AN, Bardou M, Martel M. et al. Prokinetics in acute upper GI bleeding: a meta-analysis. Gastrointest Endosc 2010;72:1138–45. - PubMed
-
- Lau JY, Leung WK, Wu JC. et al. Omeprazole before endoscopy in patients with gastrointestinal bleeding. N Engl J Med 2007;356:1631–40. - PubMed
-
- Mullady DK, Wang AY, Waschke KA.. AGA clinical practice update on endoscopic therapies for non-variceal upper gastrointestinal bleeding: expert review. Gastroenterology 2020;159:1120–8. - PubMed
-
- Tsoi KK, Lau JY, Sung JJ.. Cost-effectiveness analysis of high-dose omeprazole infusion before endoscopy for patients with upper-GI bleeding. Gastrointest Endosc 2008;67:1056–63. - PubMed
-
- Barkun AN. Should every patient with suspected upper GI bleeding receive a proton pump inhibitor while awaiting endoscopy? Gastrointest Endosc 2008;67:1064–6. - PubMed
-
- Al-Sabah S, Barkun AN, Herba K. et al. Cost-effectiveness of proton-pump inhibition before endoscopy in upper gastrointestinal bleeding. Clin Gastroenterol Hepatol 2008;6:418–25. - PubMed
-
- Laursen SB, Leontiadis GI, Stanley AJ. et al. Relationship between timing of endoscopy and mortality in patients with peptic ulcer bleeding: a nationwide cohort study. Gastrointest Endosc 2017;85:936–44.e3. - PubMed
-
- Lau JYW, Yu Y, Tang RSY. et al. Timing of endoscopy for acute upper gastrointestinal bleeding. N Engl J Med 2020;382:1299–308. - PubMed
-
- Garcia-Tsao G, Abraldes JG, Berzigotti A. et al. Portal hypertensive bleeding in cirrhosis: Risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases. Hepatology 2017;65:310–35. - PubMed
-
- Elmunzer BJ, Young SD, Inadomi JM. et al. Systematic review of the predictors of recurrent hemorrhage after endoscopic hemostatic therapy for bleeding peptic ulcers. Am J Gastroenterol 2008;103:2625–32; quiz 2633. - PubMed
-
- Laine L, Peterson WL.. Bleeding peptic ulcer. N Engl J Med 1994;331:717–27. - PubMed
-
- Laine L, McQuaid KR.. Endoscopic therapy for bleeding ulcers: an evidence-based approach based on meta-analyses of randomized controlled trials. Clin Gastroenterol Hepatol 2009;7:33–47. - PubMed
-
- Chung IK, Ham JS, Kim HS. et al. Comparison of the hemostatic efficacy of the endoscopic hemoclip method with hypertonic saline-epinephrine injection and a combination of the two for the management of bleeding peptic ulcers. Gastrointest Endosc 1999;49:13–8. - PubMed
-
- Schmidt A, Gölder S, Goetz M. et al. Over-the-scope clips are more effective than standard endoscopic therapy for patients with recurrent bleeding of peptic ulcers. Gastroenterology 2018;155:674–86.e6. - PubMed
-
- Bapaye J, Chandan S, Naing LY. et al. Safety and efficacy of over-the-scope clips versus standard therapy for high-risk nonvariceal upper GI bleeding: systematic review and meta-analysis. Gastrointest Endosc 2022;96:712–20.e7. - PubMed
-
- Barkun AN, Laine L, Leontiadis GI. et al. Over-the-scope clips versus standard treatment. Gut 2022;2022:327712. - PubMed
-
- Takizawa K, Oda I, Gotoda T. et al. Routine coagulation of visible vessels may prevent delayed bleeding after endoscopic submucosal dissection: an analysis of risk factors. Endoscopy 2008;40:179–83. - PubMed
-
- Toka B, Eminler AT, Karacaer C. et al. Comparison of monopolar hemostatic forceps with soft coagulation versus hemoclip for peptic ulcer bleeding: a randomized trial (with video). Gastrointest Endosc 2019;89:792–802. - PubMed
-
- Arima S, Sakata Y, Ogata S. et al. Evaluation of hemostasis with soft coagulation using endoscopic hemostatic forceps in comparison with metallic hemoclips for bleeding gastric ulcers: a prospective, randomized trial. J Gastroenterol 2010;45:501–5. - PubMed
-
- Kim JW, Jang JY, Lee CK. et al. Comparison of hemostatic forceps with soft coagulation versus argon plasma coagulation for bleeding peptic ulcer: a randomized trial. Endoscopy 2015;47:680–7. - PubMed
-
- Nunoue T, Takenaka R, Hori K. et al. A randomized trial of monopolar soft-mode coagulation versus heater probe thermocoagulation for peptic ulcer bleeding. J Clin Gastroenterol 2015;49:472–6. - PubMed
-
- Chen YI, Barkun AN, Soulellis C. et al. Use of the endoscopically applied hemostatic powder TC-325 in cancer-related upper GI hemorrhage: preliminary experience (with video). Gastrointest Endosc 2012;75:1278–81. - PubMed
-
- Sung JJ, Luo D, Wu JC. et al. Early clinical experience of the safety and effectiveness of Hemospray in achieving hemostasis in patients with acute peptic ulcer bleeding. Endoscopy 2011;43:291–5. - PubMed
-
- Rodríguez de Santiago E, Burgos-Santamaría D, Pérez-Carazo L. et al.; TC-325 Collaboration Project, Endoscopy Group of the Spanish Association of Gastroenterology. Hemostatic spray powder TC-325 for GI bleeding in a nationwide study: survival and predictors of failure via competing risks analysis. Gastrointest Endosc 2019;90:581–90.e6. - PubMed
-
- Chen YI, Wyse J, Lu Y. et al. TC-325 hemostatic powder versus current standard of care in managing malignant GI bleeding: a pilot randomized clinical trial. Gastrointest Endosc 2020;91:321–8.e1. - PubMed
-
- Haddara S, Jacques J, Lecleire S. et al. A novel hemostatic powder for upper gastrointestinal bleeding: a multicenter study (the "GRAPHE" registry). Endoscopy 2016;48:1084–95. - PubMed
-
- Hussein M, Alzoubaidi D, Lopez MF. et al. Hemostatic spray powder TC-325 in the primary endoscopic treatment of peptic ulcer-related bleeding: multicenter international registry. Endoscopy 2021;53:36–43. - PubMed
-
- Kwek BEA, Ang TL, Ong PLJ. et al. TC-325 versus the conventional combined technique for endoscopic treatment of peptic ulcers with high-risk bleeding stigmata: a randomized pilot study. J Dig Dis 2017;18:323–9. - PubMed
-
- Lau JYW, Pittayanon R, Kwek A. et al. Comparison of a hemostatic powder and standard treatment in the control of active bleeding from upper nonvariceal lesions: a multicenter, noninferiority, randomized trial. Ann Intern Med 2022;175:171–8. - PubMed
-
- Chen YI, Barkun AN.. Hemostatic powders in gastrointestinal bleeding: a systematic review. Gastrointest Endosc Clin N Am 2015;25:535–52. - PubMed
-
- Chen YI, Barkun A, Nolan S.. Hemostatic powder TC-325 in the management of upper and lower gastrointestinal bleeding: a two-year experience at a single institution. Endoscopy 2015;47:167–71. - PubMed
-
- Park JC, Kim YJ, Kim EH. et al. Effectiveness of the polysaccharide hemostatic powder in non-variceal upper gastrointestinal bleeding: Using propensity score matching. J Gastroenterol Hepatol 2018;33:1500–6. - PubMed
-
- Prei JC, Barmeyer C, Bürgel N. et al. EndoClot polysaccharide hemostatic system in nonvariceal gastrointestinal bleeding: results of a prospective multicenter observational pilot study. J Clin Gastroenterol 2016;50:e95–100. - PubMed
-
- de Nucci G, Reati R, Arena I. et al. Efficacy of a novel self-assembling peptide hemostatic gel as rescue therapy for refractory acute gastrointestinal bleeding. Endoscopy 2020;52:773–9. - PubMed
-
- Song H, Zhang L, Zhao X.. Hemostatic efficacy of biological self-assembling peptide nanofibers in a rat kidney model. Macromol Biosci 2010;10:33–9. - PubMed
-
- Luo Z, Wang S, Zhang S.. Fabrication of self-assembling D-form peptide nanofiber scaffold d-EAK16 for rapid hemostasis. Biomaterials 2011;32:2013–20. - PubMed
-
- Barkun AN, Adam V, Wong RCK.. Use of Doppler probe in nonvariceal upper-gastrointestinal bleeding is less costly and more effective than standard of care. Clin Gastroenterol Hepatol 2019;17:2463–70. - PubMed
-
- Leontiadis GI, Sharma VK, Howden CW.. Proton pump inhibitor treatment for acute peptic ulcer bleeding. Cochrane Database Syst Rev 2006;1:CD002094. - PubMed
-
- Tsoi KK, Hirai HW, Sung JJ.. Meta-analysis: comparison of oral vs. intravenous proton pump inhibitors in patients with peptic ulcer bleeding. Aliment Pharmacol Ther 2013;38:721–8. - PubMed
-
- Sung JJ, Suen BY, Wu JC. et al. Effects of intravenous and oral esomeprazole in the prevention of recurrent bleeding from peptic ulcers after endoscopic therapy. Am J Gastroenterol 2014;109:1005–10. - PubMed
-
- Barkun AN, Herba K, Adam V. et al. The cost-effectiveness of high-dose oral proton pump inhibition after endoscopy in the acute treatment of peptic ulcer bleeding. Aliment Pharmacol Ther 2004;20:195–202. - PubMed
-
- Hearnshaw SA, Logan RF, Lowe D. et al. Acute upper gastrointestinal bleeding in the UK: patient characteristics, diagnoses and outcomes in the 2007 UK audit. Gut 2011;60:1327–35. - PubMed
-
- Lau JY, Barkun A, Fan DM. et al. Challenges in the management of acute peptic ulcer bleeding. Lancet 2013;381:2033–43. - PubMed
-
- García-Iglesias P, Villoria A, Suarez D. et al. Meta-analysis: predictors of rebleeding after endoscopic treatment for bleeding peptic ulcer. Aliment Pharmacol Ther 2011;34:888–900. - PubMed
-
- Birda CL, Kumar A, Samanta J.. Endotherapy for nonvariceal upper gastrointestinal hemorrhage. Journal of Digestive Endoscopy 2021;12:78–92.
-
- Lau JY, Sung JJ, Lam YH. et al. Endoscopic retreatment compared with surgery in patients with recurrent bleeding after initial endoscopic control of bleeding ulcers. N Engl J Med 1999;340:751–6. - PubMed
-
- Sverdén E, Mattsson F, Lindström D. et al. Transcatheter arterial embolization compared with surgery for uncontrolled peptic ulcer bleeding: a population-based cohort study. Ann Surg 2019;269:304–9. - PubMed
-
- Lau JYW, Pittayanon R, Wong KT. et al. Prophylactic angiographic embolisation after endoscopic control of bleeding to high-risk peptic ulcers: a randomised controlled trial. Gut 2019;68:796–803. - PubMed
-
- Hopkins RJ, Girardi LS, Turney EA.. Relationship between Helicobacter pylori eradication and reduced duodenal and gastric ulcer recurrence: a review. Gastroenterology 1996;110:1244–52. - PubMed
-
- Gisbert JP, Khorrami S, Carballo F. et al. Helicobacter pylori eradication therapy vs. antisecretory non-eradication therapy for the prevention of recurrent bleeding from peptic ulcer. Aliment Pharmacol Ther 2004;19:617–29. - PubMed
-
- Barkun AN, Bardou M, Kuipers EJ. et al.; International Consensus Upper Gastrointestinal Bleeding Conference Group. International consensus recommendations on the management of patients with nonvariceal upper gastrointestinal bleeding. Ann Intern Med 2010;152:101–13. - PubMed
-
- Sverdén E, Brusselaers N, Wahlin K. et al. Time latencies of Helicobacter pylori eradication after peptic ulcer and risk of recurrent ulcer, ulcer adverse events, and gastric cancer: a population-based cohort study. Gastrointest Endosc 2018;88:242–50.e1. - PubMed
-
- Abraham NS, Barkun AN, Sauer BG. et al. American College of Gastroenterology–Canadian Association of Gastroenterology clinical practice guideline: management of anticoagulants and antiplatelets during acute gastrointestinal bleeding and the periendoscopic period. Am J Gastroenterol 2022;117:542–58. - PMC - PubMed
-
- Barkun AN, Douketis J, Noseworthy PA. et al. Management of patients on anticoagulants and antiplatelets during acute gastrointestinal bleeding and the peri-endoscopic period: a clinical practice guideline dissemination tool. Am J Gastroenterol 2022;117:513–9. - PubMed
-
- Sung JJ, Lau JY, Ching JY. et al. Continuation of low-dose aspirin therapy in peptic ulcer bleeding: a randomized trial. Ann Intern Med 2010;152:1–9. - PubMed
-
- Chan FKL, Goh KL, Reddy N. et al. Management of patients on antithrombotic agents undergoing emergency and elective endoscopy: joint Asian Pacific Association of Gastroenterology (APAGE) and Asian Pacific Society for Digestive Endoscopy (APSDE) practice guidelines. Gut 2018;67:405–17. - PMC - PubMed
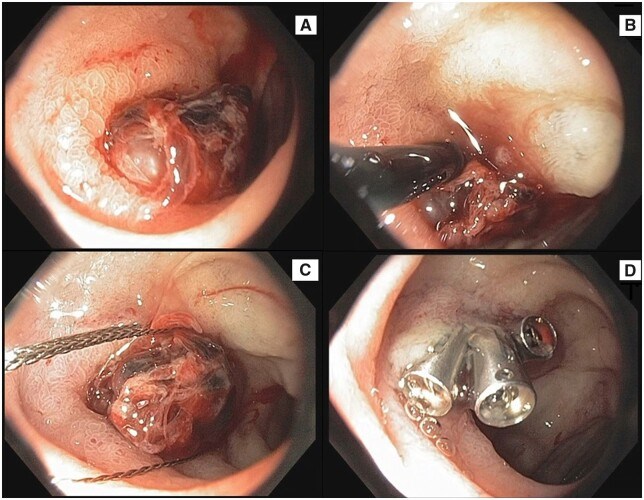
![Figure 1. The Yano–Yamamoto classification of vascular lesions (modified from the study by Yano et al. [27])](/Images/Figures/45_2438.jpeg)