Epidemiology and Outcomes from Out-of-Hospital Cardiac Arrest in Kuwait
Affiliations
Affiliations
- 1Department of Applied Medical Sciences, Health Sciences College, Public Authority of Applied Education and Training, Adailiyah, Kuwait.
- 2Audit Department, Emergency Medicals Services, Adailiyah, Kuwait.
- 3Department of Emergency Medicine, American University of Beirut Medical Center, Beirut, Lebanon.
Abstract
Background: Out-of-hospital cardiac arrest (OHCA) survival remains low in most countries. Few studies examine OHCA outcomes out of the Middle East region. This is the first study to describe characteristics and outcomes of patients with OHCA treated by emergency medical services (EMS) in regions of Kuwait.
Objectives: To describe characteristics and outcomes of adult patients affected with OHCA in regions of Kuwait.
Methods: This was a retrospective observational study on all adult OHCA patients transported by EMS to regional emergency departments over a 10- month period (21 February-31 December 2017). Data were collected from various sources: national emergency medical services archived data, emergency department, intensive care unit, and cardiac care unit of two hospitals.
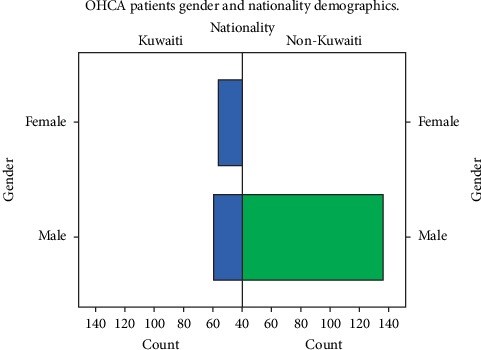
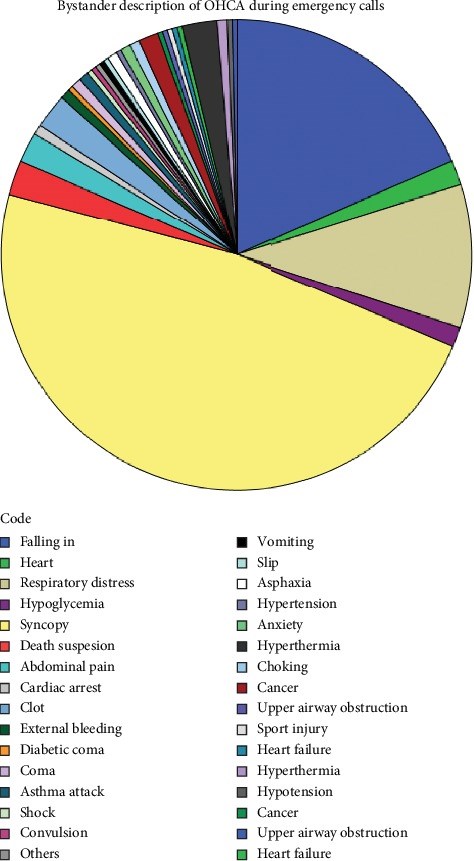
Results: A total of 332 EMS-treated OHCA cases were reviewed, and 286 incidents with OHCA from cardiac aetiology were included in the study. Most were non-Kuwaiti (60.8%) males (67.1%) with mean age 61 (+-16) years. Most OHCA cases occurred at home (76%) but with low witness rate (11.5%). Bystander CPR rate was low (8.7%). ROSC was achieved in ten patients (3.5%), but only 1 (0.3%) patient survived to hospital discharge.
Conclusion: OHCA survival rates in this region of Kuwait are low. Targeted measures such as creating cardiac registry, dispatcher-assisted CPR with ongoing training and quality improvement, and community-based CPR education program are needed to improve the survival rates of OHCA victims.
Conflict of interest statement
The authors report no conflicts of interest.
Figures
Similar articles
Hasan DA, Drennan J, Monger E, Mahmid SA, Ahmad H, Ameen M, Sayed ME.Medicine (Baltimore). 2019 Nov;98(44):e17752. doi: 10.1097/MD.0000000000017752.PMID: 31689831 Free PMC article.
McNally B, Robb R, Mehta M, Vellano K, Valderrama AL, Yoon PW, Sasson C, Crouch A, Perez AB, Merritt R, Kellermann A; Centers for Disease Control and Prevention.MMWR Surveill Summ. 2011 Jul 29;60(8):1-19.PMID: 21796098
Lee SY, Hong KJ, Shin SD, Ro YS, Song KJ, Park JH, Kong SY, Kim TH, Lee SC.Resuscitation. 2019 Feb;135:21-29. doi: 10.1016/j.resuscitation.2019.01.004. Epub 2019 Jan 9.PMID: 30639789
Zhan L, Yang LJ, Huang Y, He Q, Liu GJ.Cochrane Database Syst Rev. 2017 Mar 27;3(3):CD010134. doi: 10.1002/14651858.CD010134.pub2.PMID: 28349529 Free PMC article. Review.
Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis.
Sasson C, Rogers MA, Dahl J, Kellermann AL.Circ Cardiovasc Qual Outcomes. 2010 Jan;3(1):63-81. doi: 10.1161/CIRCOUTCOMES.109.889576. Epub 2009 Nov 10.PMID: 20123673 Review.
Cited by
Alhasan D, Fakhraldeen M, Alqabandi S, Alajmi M.Open Access Emerg Med. 2022 Nov 29;14:639-648. doi: 10.2147/OAEM.S382744. eCollection 2022.PMID: 36471824 Free PMC article.
KMEL References
References
-
- Grasner J., Lefering R., Koster R. EuReCa ONE; 27 Nations, ONE Europe, ONE Registry: a prospective one month analysis of out-of-hospital cardiac arrest outcomes in 27 countries in Europe. Resuscitation. 2016;105:188–195. - PubMed
-
- 2019. American Heart Association, Out-of-hospital Chain of Survival, American Heart association 2019, https://cpr.heart.org/AHAECC/CPRAndECC/AboutCPRFirstAid/CPRFactsAndStats....
-
- Global resuscitation alliance ‘improving survival of out- of—hospital cardiac arrest; acting on the call, Update from the Global Resuscitation Alliance, Including 27 Case Reports’ United states 2018, https://www.cercp.org/images/stories/recursos/articulos_docs_interes/doc....
-
- El Sayed M., Assad R., Abbi Aad Y., Gharios M., Refaat M., Tamim H. Measuring the impact of emergency medical services (EMS) on out-of-hospital cardiac arrest survival in a developing country; a key metric for EMS systems’ performance. Medicine. 2017;96(29):p. 7570. doi: 10.1097/md.0000000000007570. - DOI - PMC - PubMed
-
- Kuwait Emergency Medical Services Training Department. Cardiac arrest refreshment Program; instructor in field Kuwait. Kuwait Emergency Medical Services. 2015
-
- The public authority of civil information ‘distribution of the population by gender and nationality in each governorate’ Kuwait, Statistics Services System, 2017.
-
- Kuwait emergency medical services ‘operation department annual report, Kuwait; Kuwait Operation Unit 2013.
-
- Ministry of interior. General Department of Immigration. Visiting Visas’ Kuwait: Ministry of Interior; 2018.
-
- Fan K., Leung L. Prognosis of patients with ventricular fibrillation in out-of-hospital cardiac arrest in Hong Kong: prospective study. Hong Kong Medicine Journal. 2002;8:318–321. - PubMed
-
- Alnemer K., Alqumaizi K., Alnemer A., et al. Ambulance response time to cardiac emergencies in Riyadh. Imam Journal of Applied Science. 2016;1:33–38.