Expert consensus for a national essential antidote list: E-Delphi method
Affiliations
Affiliations
- 1Department of Pharmacy Practice, College of Pharmacy, Kuwait University, Jabriya, Kuwait.
- 2Pharmacist, Ministry of Health, Kuwait, Kuwait.
- 3Department of Pharmacology and Therapeutics, College of Pharmacy, Kuwait University, Jabriya, Kuwait.
Abstract
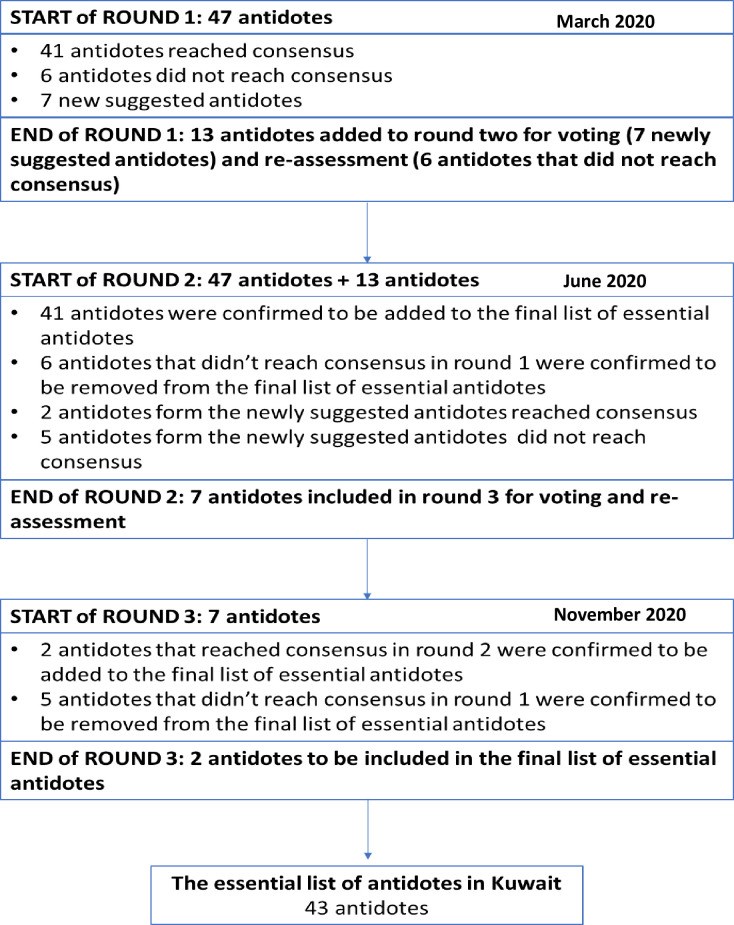
Antidote stocking represents a major challenge to hospitals all over the world, including Kuwait. In order to assist hospitals to reduce costs and improve patient care, an essential antidote list can be used as an initial foundation for securing sufficient antidote availability at healthcare institutions. The aim of our study is to generate a nationally relevant essential antidote list for emergency care hospitals in Kuwait using the e-Delphi method by establishing consensus through a multidisciplinary expert group of healthcare providers. An electronic survey with 47 essential antidotes was developed. The e-Delphi method was used, with three rounds of voting, to determine expert consensus on an essential antidote list for hospitals in Kuwait. A purposive sample of healthcare professionals from governmental and private hospitals were selected for this study (n = 30). Consensus was gained if ≥75% of the expert panel agreed on the inclusion of the antidote, without any strong disagreements. Round 1 of the e-Delphi resulted in 41 antidotes reaching consensus and seven new antidotes suggested by the expert panel. Round 2 had two antidotes (out of seven newly suggested ones) reaching consensus. Round 3 was a confirmatory round, where the expert group agreed on their previous rounds' opinions. This resulted in the development of an essential antidote list with 43 antidotes. The optimal approach for ensuring adequate availability of antidotes is continuous monitoring of local poisoning incidence and antidote requirements through collaborations between academic researchers and emergency care clinicians. The development of an essential antidote list, with expert consensus, is one of the initial steps in securing a foundation for appropriate provision of antidotes at all healthcare institutions. This is the first study that the authors are aware of that demonstrates that the e-Delphi technique can consolidate recommendations of experts in emergency medicine to provide a list of essential antidotes.
Conflict of interest statement
The authors have declared that no competing interests exist.
Figures
Similar articles
Expert Consensus Guidelines for Stocking of Antidotes in Hospitals That Provide Emergency Care.
Dart RC, Goldfrank LR, Erstad BL, Huang DT, Todd KH, Weitz J, Bebarta VS, Caravati EM, Henretig FM, Delbridge TR, Banner W, Schneider SM, Anderson VE.Ann Emerg Med. 2018 Mar;71(3):314-325.e1. doi: 10.1016/j.annemergmed.2017.05.021. Epub 2017 Jun 29.PMID: 28669553 Review.
Expert consensus guidelines for stocking of antidotes in hospitals that provide emergency care.
Dart RC, Borron SW, Caravati EM, Cobaugh DJ, Curry SC, Falk JL, Goldfrank L, Gorman SE, Groft S, Heard K, Miller K, Olson KR, O'Malley G, Seger D, Seifert SA, Sivilotti ML, Schaeffer T, Tomassoni AJ, Wise R, Bogdan GM, Alhelail M, Buchanan J, Hoppe J, Lavonas E, Mlynarchek S, Phua DH, Rhyee S, Varney S, Zosel A; Antidote Summit Authorship Group.Ann Emerg Med. 2009 Sep;54(3):386-394.e1. doi: 10.1016/j.annemergmed.2009.01.023. Epub 2009 May 5.PMID: 19406507
Availability of Antidotes in Kuwait: A National Audit.
Al-Taweel D, Al-Haqan A, Qabazard B, Abuzainah D, Koshy S, Alqenae F, Ali S, Abahussain E.J Emerg Med. 2020 Feb;58(2):305-312. doi: 10.1016/j.jemermed.2019.11.016. Epub 2019 Dec 7.PMID: 31818607
National study on the adequacy of antidotes stocking in Lebanese hospitals providing emergency care.
Mansour A, Al-Bizri L, El-Maamary J, Al-Helou A, Hamade R, Saliba E, Khammash D, Makhoul K, Matli K, Ghosn N, Deeb M, Faour WH.BMC Pharmacol Toxicol. 2016 Nov 7;17(1):51. doi: 10.1186/s40360-016-0092-7.PMID: 27817746 Free PMC article.
Dart RC, Goldfrank LR, Chyka PA, Lotzer D, Woolf AD, McNally J, Snodgrass WR, Olson KR, Scharman E, Geller RJ, Spyker D, Kraft M, Lipsy R.Ann Emerg Med. 2000 Aug;36(2):126-132. doi: 10.1067/mem.2000.108182.PMID: 10918103 Review.
KMEL References
References
- Dart RC, Goldfrank LR, Erstad BL, Huang DT, Todd KH, Weitz J, et al.. Expert Consensus Guidelines for Stocking of Antidotes in Hospitals That Provide Emergency Care. Annals of emergency medicine. 2018;71(3):314–25 e1. doi: 10.1016/j.annemergmed.2017.05.021 - DOI - PubMed
- Thanacoody RH, Aldridge G, Laing W, Dargan PI, Nash S, Thompson JP, et al.. National audit of antidote stocking in acute hospitals in the UK. Emerg Med J. 2013;30(5):393–6. doi: 10.1136/emermed-2012-201224 - DOI - PubMed
- Al-Sohaim SI, Awang R, Zyoud SH, Rashid SM, Hashim S. Evaluate the impact of hospital types on the availability of antidotes for the management of acute toxic exposures and poisonings in Malaysia. Hum Exp Toxicol. 2012;31(3):274–81. doi: 10.1177/0960327111405861 - DOI - PubMed
- Mansour A, Al-Bizri L, El-Maamary J, Al-Helou A, Hamade R, Saliba E, et al.. National study on the adequacy of antidotes stocking in Lebanese hospitals providing emergency care. BMC Pharmacol Toxicol. 2016;17(1):51. doi: 10.1186/s40360-016-0092-7 - DOI - PMC - PubMed
- Ong HC, Yang CC, Deng JF. Inadequate stocking of antidotes in Taiwan: is it a serious problem? J Toxicol Clin Toxicol. 2000;38(1):21–8. doi: 10.1081/clt-100100911 - DOI - PubMed
- Salem WA SR, Qureshi I, Al-Bukari AA, Shaat EBJ, Moinudheen J et al.. Appropriate Utilization and Stocking of Antidotes in Qatar Public Hospitals. Asia Pacific Journal of Medical Toxicology. 2017;6(3):72–8.
- AlTamimi A, Malhis NK, Khojah NM, Manea SA, AlTamimi A, AlShammary SA. Antidote Availability in Saudi Arabia Hospitals in the Riyadh Province. Basic Clin Pharmacol Toxicol. 2018;122(2):288–92. doi: 10.1111/bcpt.12897 - DOI - PubMed
- Al-Taweel D, Al-Haqan A, Qabazard B, Abuzainah D, Koshy S, Alcienae F, et al.. Availability of Antidotes in Kuwait: A National Audit. J Emerg Med. 2020;58(2):305–12. doi: 10.1016/j.jemermed.2019.11.016 - DOI - PubMed
- Marraffa JM, Cohen V, Howland MA. Antidotes for toxicological emergencies: a practical review. Am J Health Syst Pharm. 2012;69(3):199–212. doi: 10.2146/ajhp110014 - DOI - PubMed
- WHO. WHO Handbook for Guideline Development 2014 [Available from: https://apps.who.int/iris/handle/10665/145714.
- Hsu C-C SB. The Delphi Technique: Making Sense Of Consensus. Practical Assessment, Research and Evaluation. 2007;12(10).
- Sohn CH, Ryoo SM, Lim KS, Kim W, Lim H, Oh BJ. Kind and estimated stocking amount of antidotes for initial treatment for acute poisoning at emergency medical centers in Korea. J Korean Med Sci. 2014;29(11):1562–71. doi: 10.3346/jkms.2014.29.11.1562 - DOI - PMC - PubMed
- Dart RC, Goldfrank LR, Chyka PA, Lotzer D, Woolf AD, McNally J, et al.. Combined evidence-based literature analysis and consensus guidelines for stocking of emergency antidotes in the United States. Annals of emergency medicine. 2000;36(2):126–32. doi: 10.1067/mem.2000.108182 - DOI - PubMed
- O’Donnell SM CA, Adams J, Long E, Babl FE. Delphi assessment of audit and research priorities in an emergency department. Emerg Med Australas. 2020;32(4):556–61. doi: 10.1111/1742-6723.13453 - DOI - PubMed
- Donohoe H SM, Tennant B. Advantages and Limitations of the e-Delphi Technique. American Journal of Health Education. 2012;43:38–46.
- Central Statistical Bureau. Population Estimates of Kuwait 2020 [Available from: https://www.csb.gov.kw/Pages/Statistics_en?ID=67&ParentCatID=1.
- Al-Mutawa A, Abahussain E, Hedaya M, S. K. Intentional and unintentional drug poisonings in Mubarak Al-Kabeer hospital, Kuwait. J Pharma Care Health Sys. 2015;2(3).
- Al-Kandary N, Al-Waheeb S. Patterns of accidental deaths in Kuwait: a retrospective descriptive study from 2003–2009. BMC public health. 2015;15:302. doi: 10.1186/s12889-015-1630-8 - DOI - PMC - PubMed
- Abahussain EA, Ball DE. Pharmaceutical and chemical pediatric poisoning in Kuwait: a retrospective survey. Pharmacy practice. 2010;8(1):43–9. doi: 10.4321/s1886-36552010000100005 - DOI - PMC - PubMed
- Royal College of Emergency Medicine and National Poisons Information Service Guideline on Antidote Availability for Emergency Departments (2017).
- Akins RB TH, Cole BR. Stability of response characteristics of a Delphi panel: application of bootstrap data expansion. BMC Med Res Methodol. 2005;5(37). - PMC - PubMed
- James D, Warren-Forward H. Research methods for formal consensus development. Nurse researcher. 2015;22(3):35–40. doi: 10.7748/nr.22.3.35.e1297 - DOI - PubMed
- Birko S, Dove ES, Ozdemir V. Evaluation of Nine Consensus Indices in Delphi Foresight Research and Their Dependency on Delphi Survey Characteristics: A Simulation Study and Debate on Delphi Design and Interpretation. PLoS One. 2015;10(8):e0135162. doi: 10.1371/journal.pone.0135162 - DOI - PMC - PubMed
- Boulkedid R, Abdoul H, Loustau M, Sibony O, Alberti C. Using and reporting the Delphi method for selecting healthcare quality indicators: a systematic review. PLoS One. 2011;6(6):e20476. doi: 10.1371/journal.pone.0020476 - DOI - PMC - PubMed
- Diamond IR, Grant RC, Feldman BM, Pencharz PB, Ling SC, Moore AM, et al.. Defining consensus: a systematic review recommends methodologic criteria for reporting of Delphi studies. J Clin Epidemiol. 2014;67(4):401–9. doi: 10.1016/j.jclinepi.2013.12.002 - DOI - PubMed
- Foth T, Efstathiou N, Vanderspank-Wright B, Ufholz LA, Dutthorn N, Zimansky M, et al.. The use of Delphi and Nominal Group Technique in nursing education: A review. Int J Nurs Stud. 2016;60:112–20. doi: 10.1016/j.ijnurstu.2016.04.015 - DOI - PubMed
- Barrios M GG, Nuno L, Gomez-Benito J. Consensus in the delphi method: What makes a decision change? Technological Forecasting and Social Change. 2020;163.
- Keeney S, Hasson F, McKenna HP. A critical review of the Delphi technique as a research methodology for nursing. Int J Nurs Stud. 2001;38(2):195–200. doi: 10.1016/s0020-7489(00)00044-4 - DOI - PubMed
- Nasa P JR, Juneja D. Delphi methodology in healthcare research: How to decide its appropriateness. World J Methodol. 2021;11(4):116–29. doi: 10.5662/wjm.v11.i4.116 - DOI - PMC - PubMed
- Henderson EJ RG. Development of a community-based model for respiratory care services. BMC Health Serv Res 2012;12(193). doi: 10.1186/1472-6963-12-193 - DOI - PMC - PubMed
- Vogel C, Zwolinsky S., Griffiths C. et al.. A Delphi study to build consensus on the definition and use of big data in obesity research. Int J Obes 2019;43:2573–86. doi: 10.1038/s41366-018-0313-9 - DOI - PMC - PubMed
- Okoli C PS. The Delphi method as a research tool: an example, design considerations and applications. Information and Management. 2004;42:15–29.
- Marchetti A, Rossiter R. Managing acute acetaminophen poisoning with oral versus intravenous N-acetylcysteine: a provider-perspective cost analysis. J Med Econ. 2009;12(4):384–91. doi: 10.3111/13696990903435829 - DOI - PubMed
- Graham J, Traylor J. Cyanide Toxicity. StatPearls. Treasure Island (FL) 2021.
- Marrs TC, Thompson JP. The efficacy and adverse effects of dicobalt edetate in cyanide poisoning. Clin Toxicol (Phila). 2016;54(8):609–14. doi: 10.1080/15563650.2016.1186804 - DOI - PubMed
- Offerman SR, Daubert GP, Clark RF. The treatment of black widow spider envenomation with antivenin latrodectus mactans: a case series. Perm J. 2011;15(3):76–81. doi: 10.7812/tpp/10-136 - DOI - PMC - PubMed
- Murphy CM, Hong JJ, Beuhler MC. Anaphylaxis with Latrodectus antivenin resulting in cardiac arrest. J Med Toxicol. 2011;7(4):317–21. doi: 10.1007/s13181-011-0183-1 - DOI - PMC - PubMed
- Altagracia-Martínez M K-JJ, Martínez-Núñez JM, Ríos-Castañeda C, López-Naranjo F. Prussian blue as an antidote against radioactives Thallium and Cesium poisoning. Orphan Drugs: Research and Reviews. 2012;2:13–21.
- Akha AS, Rosa J 3rd, Jahr JS, Li A, Kiai K. Sugammadex: cyclodextrins, development of selective binding agents, pharmacology, clinical development, and future directions. Anesthesiol Clin. 2010;28(4):691–708. doi: 10.1016/j.anclin.2010.08.014 - DOI - PubMed
- Tomaselli GF, Mahaffey KW, Cuker A, Dobesh PP, Doherty JU, Eikelboom JW, et al.. 2017 ACC Expert Consensus Decision Pathway on Management of Bleeding in Patients on Oral Anticoagulants: A Report of the American College of Cardiology Task Force on Expert Consensus Decision Pathways. J Am Coll Cardiol. 2017;70(24):3042–67. doi: 10.1016/j.jacc.2017.09.1085 - DOI - PubMed
- Allison TA, Lin PJ, Gass JA, Chong K, Prater SJ, Escobar MA, et al.. Evaluation of the Use of Low-Dose 4-Factor Prothrombin Complex Concentrate in the Reversal of Direct Oral Anticoagulants in Bleeding Patients. J Intensive Care Med. 2020;35(9):903–8. doi: 10.1177/0885066618800657 - DOI - PubMed
- P Iskandar YH, Mokhtar N. Developing consensus in identifying challenges of undergraduate orthodontic education in Malaysian public universities using e-Delphi. Eur J Dent Educ. 2020;24:590–600. doi: 10.1111/eje.12540 - DOI - PubMed
- Msibi P.N., Mogale R., De Waal M. & Ngcobo N. Using e-Delphi to formulate and appraise the guidelines for women’s health concerns at a coal mine: A case study. Curationis. 2018;41(1), a1934. 10.4102/curationis.v41i1.1934 - DOI - PMC - PubMed
- Eubank B.H., Mohtadi N.G., Lafave M.R., Wiley J.P., Bois A.J., Boorman R.S. et al.. Using the modified Delphi method to establish clinical consensus for the diagnosis and treatment of patients with rotator cuff pathology. BMC Medical Research Methodology. 2016;16. doi: 10.1186/s12874-016-0165-8 - DOI - PMC - PubMed