A Prospective Survey of Skin Manifestations in Children With Inborn Errors of Immunity From a National Registry Over 17 Years
Affiliations
Affiliations
- Department of Pediatrics, Faculty of Medicine, Kuwait University, Kuwait City, Kuwait.
- Allergy and Clinical Immunology Unit, Pediatric Department, Al-Sabah Hospital, Kuwait City, Kuwait.
- Department of Quantitative Methods and Information Systems, College of Business Administration, Kuwait University, Kuwait City, Kuwait.
- As'ad Al-Hamad Dermatology Center, Kuwait City, Kuwait.
Abstract
Background and objectives: Reports on skin manifestations in inborn errors of immunity (IEI) are based on retrospective analysis, small series, or isolated case reports. The present prospective study aimed to determine the spectrum of skin manifestations in children with IEI and their relevance to specific molecular defects.
Materials and methods: The data were obtained from the Kuwait National Primary Immunodeficiency Disorders Registry during the period of 2004-2020.
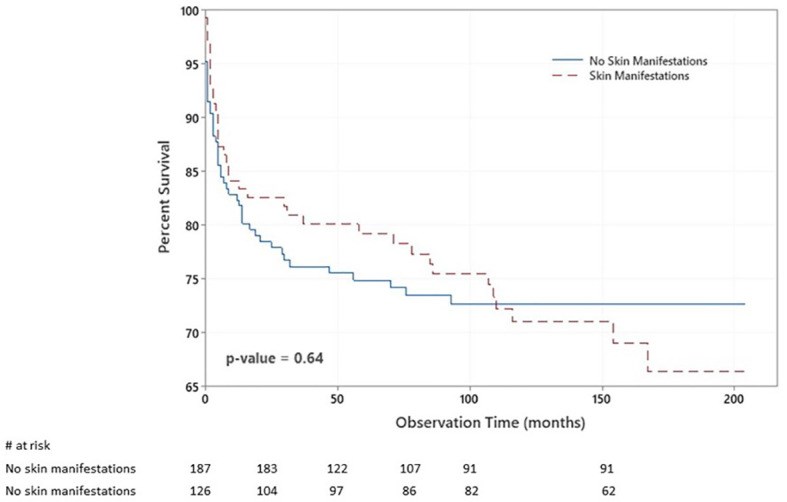
Results: A total of 313 pediatric cases of IEI, 71% diagnosed at molecular level, were registered with a cumulative follow-up period of 29,734 months. Skin manifestations were seen in 40.3% of the patients, and they were among the presenting manifestations in 33%. Patients with skin manifestations were older at both onset and diagnosis ages of IEI symptoms, but this was statistically significant for the latter only. The diagnosis delay was significantly longer in patients with skin manifestations. There was a statistically significant association between having skin manifestations and IEI category, being more common in patients with complement deficiencies, combined immunodeficiencies, and diseases of immune dysregulation. There was no statistically significant association between having skin manifestations and both gender and survival. Skin infections were the most frequent manifestations followed by eczema and autoimmune associations. Among IEI with more than 10 cases, skin lesions were a consistent finding in dedicator of cytokinesis 8 (DOCK8) deficiency, hyper IgE syndrome, ataxia-telangiectasia, and recombination activation gene (RAG)1 deficiency.
Conclusions: Skin manifestations are common in IEI patients, and they had significant diagnosis delay and referral to specialists. Improvement of awareness about IEI is needed among pediatricians and dermatologists.
Keywords: autoimmunity; cutaneous infections; eczematoid rashes; immunodeficiency; inborn errors of immunity; non-infectious cutaneous granulomas; skin manifestations.
Conflict of interest statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Figures
Similar articles
Massaad MJ, Zainal M, Al-Herz W.Front Immunol. 2020 Jun 2;11:1119. doi: 10.3389/fimmu.2020.01119. eCollection 2020.PMID: 32582199 Free PMC article.
Consensus Middle East and North Africa Registry on Inborn Errors of Immunity.
Aghamohammadi A, Rezaei N, Yazdani R, Delavari S, Kutukculer N, Topyildiz E, Ozen A, Baris S, Karakoc-Aydiner E, Kilic SS, Kose H, Gulez N, Genel F, Reisli I, Djenouhat K, Tahiat A, Boukari R, Ladj S, Belbouab R, Ferhani Y, Belaid B, Djidjik R, Kechout N, Attal N, Saidani K, Barbouche R, Bousfiha A, Sobh A, Rizk R, Elnagdy MH, Al-Ahmed M, Al-Tamemi S, Nasrullayeva G, Adeli M, Al-Nesf M, Hassen A, Mehawej C, Irani C, Megarbane A, Quinn J; MENA-I. E. I. Study Group; Maródi L, Modell V, Modell F, Al-Herz W, Geha RS, Abolhassani H.J Clin Immunol. 2021 Aug;41(6):1339-1351. doi: 10.1007/s10875-021-01053-z. Epub 2021 May 29.PMID: 34052995 Free PMC article.
Thalhammer J, Kindle G, Nieters A, Rusch S, Seppänen MRJ, Fischer A, Grimbacher B, Edgar D, Buckland M, Mahlaoui N, Ehl S; European Society for Immunodeficiencies Registry Working Party.J Allergy Clin Immunol. 2021 Nov;148(5):1332-1341.e5. doi: 10.1016/j.jaci.2021.04.015. Epub 2021 Apr 23.PMID: 33895260
Beyond Infections: New Warning Signs for Inborn Errors of Immunity in Children.
Costagliola G, Peroni DG, Consolini R.Front Pediatr. 2022 Jun 10;10:855445. doi: 10.3389/fped.2022.855445. eCollection 2022.PMID: 35757131 Free PMC article. Review.
Dendritic cells in inborn errors of immunity.
Gupta S, Agrawal A.Front Immunol. 2023 Jan 23;14:1080129. doi: 10.3389/fimmu.2023.1080129. eCollection 2023.PMID: 36756122 Free PMC article. Review.
Cited by
Atopic Dermatitis-like Genodermatosis: Disease Diagnosis and Management.
Pan C, Zhao A, Li M.Diagnostics (Basel). 2022 Sep 9;12(9):2177. doi: 10.3390/diagnostics12092177.PMID: 36140582 Free PMC article. Review.
KMEL References
References
-
- Moin A, Harhoudi A, Moin M, PourPpak Z, Bazargan N. Cutaneous Manifestations of Primary Immunodeficiency Diseases in Children. Iran J Allergy Asthma Immunol (2006) 5(3):121–6. - PubMed
-
- López-Qintero W, Cleves D, Gomez-Vasco J, Pérez P, Patiño J, Medina valencia D, et al. . Skin Manifestations in Pediatric Patients With Primary Immunodeficiency Diseases (PIDs) in a Tertiary Care Hospital in Colombia. World Allergy Organ J (2021) 14(3):e100527. doi: 10.1016/j.waojou.2021.100527 - DOI - PMC - PubMed
-
- Tangye SG, Al-Herz W, Bousfiha A, Chatila T, Cunnigham Rundles C, Etzioni A, et al. . Human Inborn Errors of Immunity 2019 Update on the Classification From the International Union of Immunological Societies Expert Committee. J Clin Immunol (2020) 40(1):24–64. doi: 10.1007/s10875-019-00737-x - DOI - PMC - PubMed