Blood biomarkers as predictors of long-term mortality in COPD
Affiliations
Affiliations
- Department of Epidemiology, College of Public Health, University of Iowa, Iowa City, Iowa.
- Division of Pediatric Pulmonary Medicine, Allergy, and Immunology, Children's Hospital of Pittsburgh of UPMC, University of Pittsburgh, Pittsburgh, Pennsylvania.
- Centre for Population Health Research, School of Health Sciences, University of South Australia, Adelaide, South Australia, Australia.
- Department of Environmental & Occupational Health, Faculty of Public Health, Kuwait University, Jabriya, Kuwait.
Abstract
Background: Blood biomarkers are easily accessible and might reflect chronic obstructive pulmonary disease (COPD) activity.
Aim: The aim of this study was to determine whether a panel of blood biomarkers [C-reactive protein (CRP), neutrophils, eosinophils, albumin and vitamin D] could predict mortality in COPD.
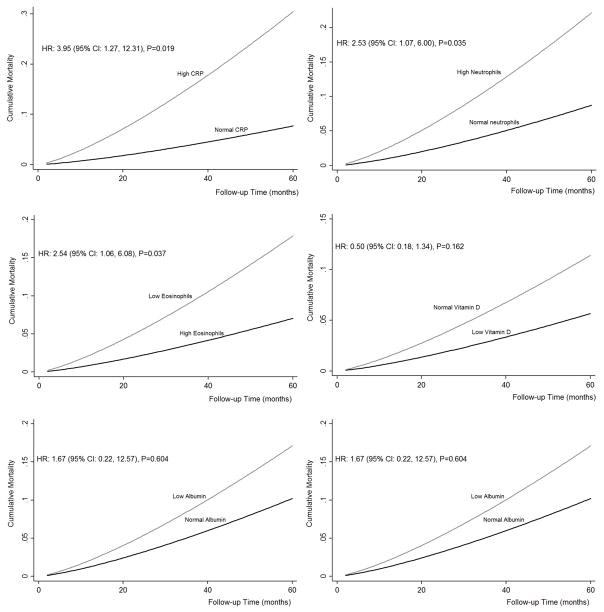
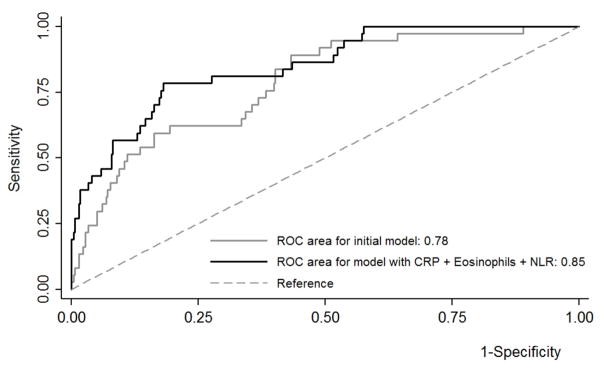
Methods: We analyzed data from 431 COPD participants to the 2007-2010 National Health and Nutrition Examination Surveys who were followed for a median time of 36 months. COPD was defined as post-bronchodilator forced expiratory volume in 1 second (FEV1) and forced vital capacity ratio <0.70. Weibull survival analysis adjusted for covariates was performed to calculate the risk of mortality associated with the biomarkers, and C-statistics was used to assess their added predictive value.
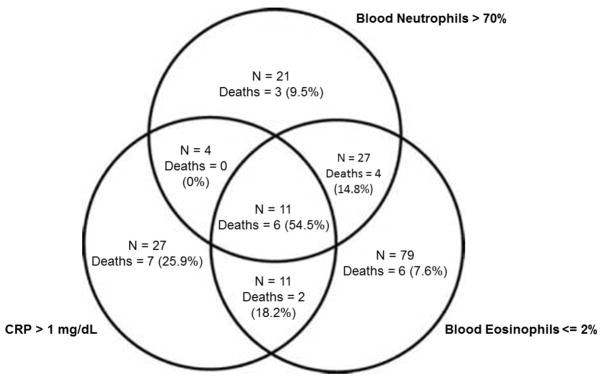
Results: During follow-up, 38 of the 431 participants died. Participants with high CRP, eosinophil count <2%, hypoalbuminemia and hypovitaminosis D had worse baseline FEV1 and subsequently higher mortality compared to controls. In adjusted analysis, increasing CRP [hazard ratio (HR): 4.45, 95% CI: 1.91-10.37] and neutrophil count (HR: 1.07, 95% CI: 1.03-1.11) as well as decreasing eosinophil count (HR: 7.03, 95% CI: 2.05-24.01) were associated with an increased risk of mortality. The addition of CRP with eosinophil and/or neutrophil count significantly improved a base model for the prediction of mortality which included age, gender, race/ethnicity, body mass index, smoking, poverty income ratio, asthma, diabetes, hypertension and history of stroke or myocardial infarction.
Conclusion: High CRP and neutrophils as well as low eosinophils are predictive of poor COPD prognosis. They also add significant value to prediction models of mortality in COPD.
Keywords: biologic markers; chronic obstructive pulmonary disease; prognosis.
Conflict of interest statement
Declaration of interests: The authors have indicated that they have no financial relationships relevant to this article to disclose. Dr. Forno’s contribution was partly funded by grant HL125666 from the U.S. NIH.
Figures
Similar articles
Inflammatory biomarkers and exacerbations in chronic obstructive pulmonary disease.
Thomsen M, Ingebrigtsen TS, Marott JL, Dahl M, Lange P, Vestbo J, Nordestgaard BG.JAMA. 2013 Jun 12;309(22):2353-61. doi: 10.1001/jama.2013.5732.PMID: 23757083
Can we predict the prognosis of COPD with a routine blood test?
Xiong W, Xu M, Zhao Y, Wu X, Pudasaini B, Liu JM.Int J Chron Obstruct Pulmon Dis. 2017 Feb 13;12:615-625. doi: 10.2147/COPD.S124041. eCollection 2017.PMID: 28243079 Free PMC article.
Prevalence and features of asthma-COPD overlap in the United States 2007-2012.
Mendy A, Forno E, Niyonsenga T, Carnahan R, Gasana J.Clin Respir J. 2018 Aug;12(8):2369-2377. doi: 10.1111/crj.12917.PMID: 29873189 Free PMC article.
Palliative care and prognosis in COPD: a systematic review with a validation cohort.
Almagro P, Yun S, Sangil A, Rodríguez-Carballeira M, Marine M, Landete P, Soler-Cataluña JJ, Soriano JB, Miravitlles M.Int J Chron Obstruct Pulmon Dis. 2017 Jun 9;12:1721-1729. doi: 10.2147/COPD.S135657. eCollection 2017.PMID: 28652724 Free PMC article. Review.
C-reactive protein level predicts mortality in COPD: a systematic review and meta-analysis.
Leuzzi G, Galeone C, Taverna F, Suatoni P, Morelli D, Pastorino U.Eur Respir Rev. 2017 Jan 31;26(143):160070. doi: 10.1183/16000617.0070-2016. Print 2017 Jan.PMID: 28143876 Free PMC article. Review.
Cited by
Ling M, Huiyin L, Shanglin C, Haiming L, Zhanyi D, Shuchun W, Meng B, Murong L.Front Med (Lausanne). 2023 Apr 27;10:1109910. doi: 10.3389/fmed.2023.1109910. eCollection 2023.PMID: 37181348 Free PMC article.
Biswas M, Suvarna R, Krishnan S V, Devasia T, Shenoy Belle V, Prabhu K.F1000Res. 2022 Aug 19;11:960. doi: 10.12688/f1000research.123245.1. eCollection 2022.PMID: 36619602 Free PMC article. Review.
Khatib S, Sabobeh T, Jaber F, Abdalla K, Singh S, Salzman G.Mo Med. 2022 Nov-Dec;119(6):545-552.PMID: 36588649 Free PMC article. Review.
Clinical Implications of Low Absolute Blood Eosinophil Count in the SPIROMICS COPD Cohort.
LeMaster WB, Quibrera PM, Couper D, Tashkin DP, Bleecker ER, Doerschuk CM, Ortega VE, Cooper C, Han MK, Woodruff PG, O'Neal WK, Anderson WH, Alexis NE, Bowler RP, Barr RG, Kaner RJ, Dransfield MT, Paine R 3rd, Kim V, Curtis JL, Martinez FJ, Hastie AT, Barjaktarevic I.Chest. 2023 Mar;163(3):515-528. doi: 10.1016/j.chest.2022.10.029. Epub 2022 Nov 4.PMID: 36343688
Mendy A, Merianos AL, Mersha TB, Mahabee-Gittens EM.Eur Respir J. 2022 Nov 17;60(5):2201185. doi: 10.1183/13993003.01185-2022. Print 2022 Nov.PMID: 36202413 No abstract available.