Spectrum of Viral Infections Among Primary Immunodeficient Children: Report From a National Registry
Affiliations
Affiliations
- Department of Pediatrics, Faculty of Medicine, Kuwait University, Kuwait City, Kuwait.
- Allergy and Clinical Immunology Unit, Pediatric Department, Al-Sabah Hospital, Kuwait City, Kuwait.
- Department of Microbiology, Faculty of Medicine, Kuwait University, Kuwait City, Kuwait.
Abstract
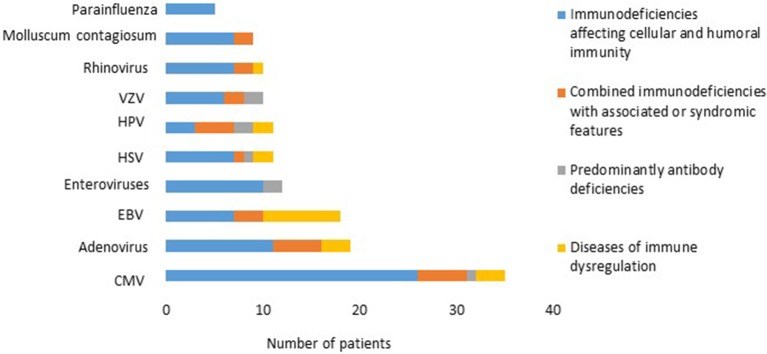
Objective: To present the frequency and spectrum of viral infections in primary immunodeficient children. Methods: The data was obtained from the Kuwait National Primary Immunodeficiency Disorders (PIDs) Registry during the period of 2004-2018. Results: A total of 274 PID children were registered in KNPIDR during the study period with predominance of immunodeficiencies affecting cellular and humoral immunity, followed by combined immunodeficiencies with associated syndromic features and diseases of immune dysregulation. Overall infectious complications affected 82.4% of the patients, and viral infections affected 31.7% of the registered patients. Forty-five patients (16.4%) developed viral infections caused by at least 2 organisms, among those 20 patients were affected by three or more viral infections. There was a statistically significant association between viral infections and PID category. However, there was no statistically significant association between viral infections and gender or the patients' onset age. There was a total of 170 viral infections during the study period and the causes of these infections were predominated by CMV (22.2%), adenovirus (11.7%), EBV (11.1%), and enteroviruses (7.4%). CMV and parainfluenza infections were more common in the group of immunodeficiencies affecting cellular and humoral immunity while EBV and human papilloma virus (HPV) were more common in the immune dysregulation group and combined immunodeficiencies with associated syndromic features, respectively. The most common presentation was viremia (28.8%) followed by pneumonia (28.2%) and skin infections (17.6%). The most common causes of viremia were CMV followed by adenovirus and EBV, while the most common organisms causing pneumonia were CMV followed by rhinovirus and parainfluenza. There were 80 deaths among the registered patients, 10% were caused by viral infections. Conclusions: Viral infections are common in PIDs and result into a wide-range of clinical manifestations causing significant morbidity and mortality.
Keywords: CMV; EBV; adenovirus; mortality; pneumonia; primary immunodeficiencies; viremia; virus.
Figures
Similar articles
Massaad MJ, Zainal M, Al-Herz W.Front Immunol. 2020 Jun 2;11:1119. doi: 10.3389/fimmu.2020.01119. eCollection 2020.PMID: 32582199 Free PMC article.
The Kuwait National Primary Immunodeficiency Registry 2004-2018.
Al-Herz W, Al-Ahmad M, Al-Khabaz A, Husain A, Sadek A, Othman Y.Front Immunol. 2019 Jul 24;10:1754. doi: 10.3389/fimmu.2019.01754. eCollection 2019.PMID: 31396239 Free PMC article. Clinical Trial.
Al-Herz W, Zainal M, Nanda A.Front Immunol. 2021 Sep 30;12:751469. doi: 10.3389/fimmu.2021.751469. eCollection 2021.PMID: 34659256 Free PMC article.
Report of the Tunisian Registry of Primary Immunodeficiencies: 25-Years of Experience (1988-2012).
Mellouli F, Mustapha IB, Khaled MB, Besbes H, Ouederni M, Mekki N, Ali MB, Larguèche B, Hachicha M, Sfar T, Gueddiche N, Barsaoui S, Sammoud A, Boussetta K, Becher SB, Meherzi A, Guandoura N, Boughammoura L, Harbi A, Amri F, Bayoudh F, Jaballah NB, Tebib N, Bouaziz A, Mahfoudh A, Aloulou H, Mansour LB, Chabchoub I, Boussoffara R, Chemli J, Bouguila J, Hassayoun S, Hammami S, Habboul Z, Hamzaoui A, Ammar J, Barbouche MR, Bejaoui M.J Clin Immunol. 2015 Nov;35(8):745-53. doi: 10.1007/s10875-015-0206-9. Epub 2015 Oct 13.PMID: 26464197 Review.
Cytomegalovirus in primary immunodeficiency.
Godsell J, Chan S, Slade C, Bryant V, Douglass JA, Sasadeusz J, Yong MK.Curr Opin Infect Dis. 2021 Dec 1;34(6):663-671. doi: 10.1097/QCO.0000000000000797.PMID: 34608876 Review.
Cited by
Pathogen-specific T Cells: Targeting Old Enemies and New Invaders in Transplantation and Beyond.
Papadopoulou A, Alvanou M, Karavalakis G, Tzannou I, Yannaki E.Hemasphere. 2023 Jan 9;7(1):e809. doi: 10.1097/HS9.0000000000000809. eCollection 2023 Jan.PMID: 36698615 Free PMC article. Review.
Essa S, Shamsah M, Alsarraf AH, Esmaeil A, Al-Shammasi A, Raghupathy R.Microorganisms. 2022 Nov 4;10(11):2194. doi: 10.3390/microorganisms10112194.PMID: 36363785 Free PMC article.
Febrile illness in high-risk children: a prospective, international observational study.
van der Velden FJS, de Vries G, Martin A, Lim E, von Both U, Kolberg L, Carrol ED, Khanijau A, Herberg JA, De T, Galassini R, Kuijpers TW, Martinón-Torres F, Rivero-Calle I, Vermont CL, Hagedoorn NN, Pokorn M, Pollard AJ, Schlapbach LJ, Tsolia M, Elefhteriou I, Yeung S, Zavadska D, Fink C, Voice M, Zenz W, Kohlmaier B, Agyeman PKA, Usuf E, Secka F, de Groot R, Levin M, van der Flier M, Emonts M; PERFORM consortium.Eur J Pediatr. 2023 Feb;182(2):543-554. doi: 10.1007/s00431-022-04642-1. Epub 2022 Oct 15.PMID: 36243780 Free PMC article.
Talaromyces marneffei Infections in 8 Chinese Children with Inborn Errors of Immunity.
Wang L, Luo Y, Li X, Li Y, Xia Y, He T, Huang Y, Xu Y, Yang Z, Ling J, Weng R, Zhu X, Qi Z, Yang J.Mycopathologia. 2022 Dec;187(5-6):455-467. doi: 10.1007/s11046-022-00659-0. Epub 2022 Sep 30.PMID: 36180657 Free PMC article.
SARS-CoV-2 infection in patients with inborn errors of immunity due to DNA repair defects.
Wang Y, Abolhassani H, Hammarström L, Pan-Hammarström Q.Acta Biochim Biophys Sin (Shanghai). 2022 Jun 25;54(6):836-846. doi: 10.3724/abbs.2022071.PMID: 35713311 Free PMC article. Review.
KMEL References
References
-
- Ljungman P, Gleaves CA, Meyers JD. Respiratory virus infection in immunocompromised patients. Bone Marrow Transplant. (1989) 4:35–40. - PubMed
-
- Medical Advisory Committee of the Immune Deficiency Foundation. Shearer WT, Fleisher TA, Buckley RH, Ballas Z, Ballow M, et al. . Recommendations for live viral and bacterial vaccines in immunodeficient patients and their close contacts. J Allergy Clin Immunol. (2014) 133:961–6. 10.1016/j.jaci.2013.11.043 - DOI - PMC - PubMed