Lactose intolerance and gastrointestinal cow's milk allergy in infants and children - common misconceptions revisited
Affiliations
Affiliations
- Murdoch Childrens Research Institute, Melbourne, Australia.
- Al Adan Hospital, Ministry of Health, Kuwait City, Kuwait.
- Rainbow Children's Hospital, Banjara Hills, Hyderabad, India.
- Philippine Society of Allergy, Asthma & Immunology, Philippine Medical Association, Quezon City, Philippines.
- Guangzhou Women and Children's Medical Center, Guangzhou Medical University, Guangzhou, China.
- Universidad National Autonoma de México, Hospital Infantil Privado Star Médica, Polanco, Mexico City, Mexico.
- Chualalongkorn University, Bangkok, Thailand.
- KK Women's and Children's Hospital and Yong Loo Lin School of Medicine and Duke-NUS Medical School, Singapore, Singapore.
- University of the Philippines, Philippine General Hospital, Manila, Philippines.
Abstract
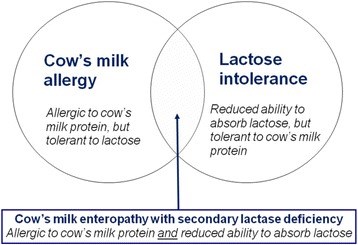
Lactose is the main carbohydrate in human and mammalian milk. Lactose requires enzymatic hydrolysis by lactase into D-glucose and D-galactose before it can be absorbed. Term infants express sufficient lactase to digest about one liter of breast milk daily. Physiological lactose malabsorption in infancy confers beneficial prebiotic effects, including the establishment of Bifidobacterium-rich fecal microbiota. In many populations, lactase levels decline after weaning (lactase non-persistence; LNP). LNP affects about 70% of the world's population and is the physiological basis for primary lactose intolerance (LI). Persistence of lactase beyond infancy is linked to several single nucleotide polymorphisms in the lactase gene promoter region on chromosome 2. Primary LI generally does not manifest clinically before 5 years of age. LI in young children is typically caused by underlying gut conditions, such as viral gastroenteritis, giardiasis, cow's milk enteropathy, celiac disease or Crohn's disease. Therefore, LI in childhood is mostly transient and improves with resolution of the underlying pathology. There is ongoing confusion between LI and cow's milk allergy (CMA) which still leads to misdiagnosis and inappropriate dietary management. In addition, perceived LI may cause unnecessary milk restriction and adverse nutritional outcomes. The treatment of LI involves the reduction, but not complete elimination, of lactose-containing foods. By contrast, breastfed infants with suspected CMA should undergo a trial of a strict cow's milk protein-free maternal elimination diet. If the infant is not breastfed, an extensively hydrolyzed or amino acid-based formula and strict cow's milk avoidance are the standard treatment for CMA. The majority of infants with CMA can tolerate lactose, except when an enteropathy with secondary lactase deficiency is present.
Keywords: Carbohydrate; Celiac disease; Cow’s milk allergy; Enteropathy; Gastroenteritis; Malabsorption.
Conflict of interest statement
Not required.All authors have reviewed the manuscript and have provided their consent for publication.Dr. Ralf Heine has been a member of the scientific advisory boards of Nestlé Health Science / Nestlé Nutrition Institute, Australia/Oceania and Nutricia Australia. He has received honoraria from industry for educational activities. All authors have received reimbursement for travel expenses for this project from Nestlé Health Science, Switzerland. The authors otherwise declare that they have no competing interests.Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Figures
Similar articles
Formulas containing hydrolysed protein for prevention of allergy and food intolerance in infants.
Osborn DA, Sinn J.Cochrane Database Syst Rev. 2006 Oct 18;(4):CD003664. doi: 10.1002/14651858.CD003664.pub3.PMID: 17054180 Updated. Review.
Formulas containing hydrolysed protein for prevention of allergy and food intolerance in infants.
Osborn DA, Sinn J.Cochrane Database Syst Rev. 2003;(4):CD003664. doi: 10.1002/14651858.CD003664.PMID: 14583987 Updated. Review.
Rectal bleeding in infancy: clinical, allergological, and microbiological examination.
Arvola T, Ruuska T, Keränen J, Hyöty H, Salminen S, Isolauri E.Pediatrics. 2006 Apr;117(4):e760-8. doi: 10.1542/peds.2005-1069.PMID: 16585287 Clinical Trial.
Bahbah WA, ElHodhod M, Salah M, AlRefaee F, AlTuraiki M, Mousa S, Al Mehaidib A, Ayesh WH, El-Bazzar AN, El Haddad J, El Khashab HY, El Zawahry A, Hasosah M, Shaaban SY, Vandenplas Y.Nutrients. 2022 Mar 3;14(5):1067. doi: 10.3390/nu14051067.PMID: 35268042 Free PMC article.
Kansu A, Yüce A, Dalgıç B, Şekerel BE, Çullu-Çokuğraş F, Çokuğraş H.Turk J Pediatr. 2016;58(1):1-11. doi: 10.24953/turkjped.2016.01.001.PMID: 27922230
Cited by
Plant-Based Dairy Alternatives-A Future Direction to the Milky Way.
Plamada D, Teleky BE, Nemes SA, Mitrea L, Szabo K, Călinoiu LF, Pascuta MS, Varvara RA, Ciont C, Martău GA, Simon E, Barta G, Dulf FV, Vodnar DC, Nitescu M.Foods. 2023 May 3;12(9):1883. doi: 10.3390/foods12091883.PMID: 37174421 Free PMC article. Review.
Food intolerances in children and adolescents in Switzerland.
Légeret C, Lohmann C, Furlano RI, Köhler H.Eur J Pediatr. 2023 Feb;182(2):867-875. doi: 10.1007/s00431-022-04755-7. Epub 2022 Dec 13.PMID: 36512149 Free PMC article.
da Silva AT, de Lima JJ, Reis P, Passos M, Baumgartner CG, Sereno AB, Krüger CCH, Cândido LMB.Foods. 2022 Nov 29;11(23):3861. doi: 10.3390/foods11233861.PMID: 36496669 Free PMC article.
Cow's milk-induced gastrointestinal disorders: From infancy to adulthood.
Al-Beltagi M, Saeed NK, Bediwy AS, Elbeltagi R.World J Clin Pediatr. 2022 Nov 9;11(6):437-454. doi: 10.5409/wjcp.v11.i6.437. eCollection 2022 Nov 9.PMID: 36439902 Free PMC article.
The Role of the Gut Microbiome in Cow's Milk Allergy: A Clinical Approach.
Moriki D, Francino MP, Koumpagioti D, Boutopoulou B, Rufián-Henares JÁ, Priftis KN, Douros K.Nutrients. 2022 Oct 28;14(21):4537. doi: 10.3390/nu14214537.PMID: 36364799 Free PMC article. Review.
KMEL References
References
-
- Wahlqvist ML. Lactose nutrition in lactase nonpersisters. Asia Pac J Clin Nutr. 2015;24(Suppl 1):S21–S25. - PubMed
-
- Harvey CB, Hollox EJ, Poulter M, Wang Y, Rossi M, Auricchio S, Iqbal TH, Cooper BT, Barton R, Sarner M, Korpela R, Swallow DM. Lactase haplotype frequencies in Caucasians: association with the lactase persistence/non-persistence polymorphism. Ann Hum Genet. 1998;62:215–223. doi: 10.1046/j.1469-1809.1998.6230215.x. - DOI - PubMed
-
- Allentoft ME, Sikora M, Sjögren KG, Rasmussen S, Rasmussen M, Stenderup J, Damgaard PB, Schroeder H, Ahlström T, Vinner L, Malaspinas AS, Margaryan A, Higham T, Chivall D, Lynnerup N, Harvig L, Baron J, Della Casa P, Dabrowski P, Duffy PR, Ebel AV, Epimakhov A, Frei K, Furmanek M, Gralak T, Gromov A, Gronkiewicz S, Grupe G, Hajdu T, Jarysz R, Khartanovich V, Khokhlov A, Kiss V, Kolář J, Kriiska A, Lasak I, Longhi C, McGlynn G, Merkevicius A, Merkyte I, Metspalu M, Mkrtchyan R, Moiseyev V, Paja L, Palfi G, Pokutta D, Pospieszny Ł, Price TD, Saag L, Sablin M, Shishlina N, Smrčka V, Soenov VI, Szeverényi V, Tóth G, Trifanova SV, Varul L, Vicze M, Yepiskoposyan L, Zhitenev V, Orlando L, Sicheritz-Pontén T, Brunak S, Nielsen R, Kristiansen K, Willerslev E. Population genomics of Bronze Age Eurasia. Nature. 2015;522:167–172. doi: 10.1038/nature14507. - DOI - PubMed
-
- Lebenthal E, Antonowicz I, Shwachman H. Correlation of lactase activity, lactose tolerance and milk consumption in different age groups. Am J Clin Nutr. 1975;28:595–600. - PubMed
-
- Welsh JD, Poley JR, Bhatia M, Stevenson DE. Intestinal disaccharidase activities in relation to age, race, and mucosal damage. Gastroenterology. 1978;75:847–855. - PubMed
-
- Grimheden P, Anderlid BM, Gåfvels M, Svahn J, Grahnquist L. Lactose intolerance in children is an overdiagnosed condition. Risk of missing intestinal diseases such as IBD and celiac disease. Läkartidningen. 2012;109:218–21. - PubMed
-
- Dahlqvist A, Hammond JB, Crane RK, Dunphy JV, Littman A. Intestinal lactase deficiency and lactose intolerance in adults. Preliminary Report Gastroenterology. 1963;45:488–491. - PubMed
-
- Auricchio S, Rubino A, Muerset G. Intestinal glycosidase activities in the human embryo, fetus, and newborn. Pediatrics. 1965;35:944–954. - PubMed
-
- Norén O, Sjöström H. Structure, biosynthesis and regulation of lactase-phlorizin hydrolase. Scand J Nutr. 2001;45:156–160.
-
- Bond JH, Levitt MD. Quantitative measurement of lactose absorption. Gastroenterology. 1976;70:1058–1062. - PubMed
-
- Hertzler SR, Savaiano DA. Colonic adaptation to daily lactose feeding in lactose maldigesters reduces lactose intolerance. Am J Clin Nutr. 1996;64:232–236. - PubMed
-
- Antonowicz I, Lebenthal E. Developmental pattern of small intestinal enterokinase and disaccharidase activities in the human fetus. Gastroenterology. 1977;72:1299–1303. - PubMed
-
- Buller HA, Van Wassenaer AG, Raghavan S, Montgomery RK, Sybicki MA, Grand RJ. New insights into lactase and glycosylceramidase activities of rat lactase-phlorizin hydrolase. Am J Phys. 1989;257:G616–G623. - PubMed
-
- Bulhoes AC, Goldani HA, Oliveira FS, Matte US, Mazzuca RB, Silveira TR. Correlation between lactose absorption and the C/T-13910 and G/A-22018 mutations of the lactase-phlorizin hydrolase (LCT) gene in adult-type hypolactasia. Braz J Med Biol Res. 2007;40:1441–1446. doi: 10.1590/S0100-879X2007001100004. - DOI - PubMed
-
- Kuchay RA, Anwar M, Thapa BR, Mahmood A, Mahmood S. Correlation of G/a −22018 single-nucleotide polymorphism with lactase activity and its usefulness in improving the diagnosis of adult-type hypolactasia among north Indian children. Genes Nutr. 2013;8:145–151. doi: 10.1007/s12263-012-0305-7. - DOI - PMC - PubMed
-
- Enattah NS, Jensen TG, Nielsen M, Lewinski R, Kuokkanen M, Rasinpera H, El-Shanti H, Seo JK, Alifrangis M, Khalil IF, Natah A, Ali A, Natah S, Comas D, Mehdi SQ, Groop L, Vestergaard EM, Imtiaz F, Rashed MS, Meyer B, Troelsen J, Peltonen L. Independent introduction of two lactase-persistence alleles into human populations reflects different history of adaptation to milk culture. Am J Hum Genet. 2008;82:57–72. doi: 10.1016/j.ajhg.2007.09.012. - DOI - PMC - PubMed
-
- Tishkoff SA, Reed FA, Ranciaro A, Voight BF, Babbitt CC, Silverman JS, Powell K, Mortensen HM, Hirbo JB, Osman M, Ibrahim M, Omar SA, Lema G, Nyambo TB, Ghori J, Bumpstead S, Pritchard JK, Wray GA, Deloukas P. Convergent adaptation of human lactase persistence in Africa and Europe. Nat Genet. 2007;39:31–40. doi: 10.1038/ng1946. - DOI - PMC - PubMed
-
- Scrimshaw NS, Murray EB. The acceptability of milk and milk products in populations with a high prevalence of lactose intolerance. Am J Clin Nutr. 1988;48:1079–1159. - PubMed
-
- Abrams SA, Griffin IJ, Davila PM. Calcium and zinc absorption from lactose-containing and lactose-free infant formulas. Am J Clin Nutr. 2002;76:442–446. - PubMed
-
- Francavilla R, Calasso M, Calace L, Siragusa S, Ndagijimana M, Vernocchi P, Brunetti L, Mancino G, Tedeschi G, Guerzoni E, Indrio F, Laghi L, Miniello VL, Gobbetti M, De Angelis M. Effect of lactose on gut microbiota and metabolome of infants with cow's milk allergy. Pediatr Allergy Immunol. 2012;23:420–427. doi: 10.1111/j.1399-3038.2012.01286.x. - DOI - PubMed
-
- West CE, Renz H, Jenmalm MC, Kozyrskyj AL, Allen KJ, Vuillermin P, Prescott SL, in-FLAME Microbiome Interest Group. The gut microbiota and inflammatory noncommunicable diseases: associations and potentials for gut microbiota therapies. J Allergy Clin Immunol 2015;135:3–13. - PubMed
-
- Tan-Dy CR, Ohlsson A. Lactase treated feeds to promote growth and feeding tolerance in preterm infants. Cochrane Database Syst Rev. 2005:CD004591. - PubMed
-
- Hegar B, Widodo A. Lactose intolerance in Indonesian children. Asia Pac J Clin Nutr. 2015;24(Suppl 1):S31–S40. - PubMed
-
- Savaiano DA, Boushey CJ, McCabe GP. Lactose intolerance symptoms assessed by meta-analysis: a grain of truth that leads to exaggeration. J Nutr. 2006;136:1107–1113. - PubMed
-
- Staudacher HM, Whelan K, Irving PM, Lomer MC. Comparison of symptom response following advice for a diet low in fermentable carbohydrates (FODMAPs) versus standard dietary advice in patients with irritable bowel syndrome. J Hum Nutr Diet. 2011;24:487–495. doi: 10.1111/j.1365-277X.2011.01162.x. - DOI - PubMed
-
- Glatstein M, Reif S, Scolnik D, Rom L, Yerushalmy-Feler A, Dali-Levy M, Cohen S. Lactose breath test in children: relationship between symptoms during the test and test results. Am J Ther. 2016; epub ahead of print. - PubMed
-
- Montalto M, Gallo A, Santoro L, D'Onofrio F, Curigliano V, Covino M, Cammarota G, Grieco A, Gasbarrini A, Gasbarrini G. Low-dose lactose in drugs neither increases breath hydrogen excretion nor causes gastrointestinal symptoms. Aliment Pharmacol Ther. 2008;28:1003–1012. doi: 10.1111/j.1365-2036.2008.03815.x. - DOI - PubMed
-
- Sanders SW, Tolman KG, Reitberg DP. Effect of a single dose of lactase on symptoms and expired hydrogen after lactose challenge in lactose-intolerant subjects. Clin Pharm. 1992;11:533–538. - PubMed
-
- Medow MS, Thek KD, Newman LJ, Berezin S, Glassman MS, Schwarz SM. Beta-galactosidase tablets in the treatment of lactose intolerance in pediatrics. Am J Dis Child. 1990;144:1261–1264. - PubMed
-
- Cochet B, Jung A, Griessen M, Bartholdi P, Schaller P, Donath A. Effects of lactose on intestinal calcium absorption in normal and lactase-deficient subjects. Gastroenterology. 1983;84:935–940. - PubMed