In-hospital mortality in SARS-CoV-2 stratified by gamma-glutamyl transferase levels
Affiliations
Affiliations
- Department of Infectious Diseases, Infectious Diseases Hospital, Shuwaikh Medical Area, Kuwait.
- Department of Cardiology, Sabah Al Ahmed Cardiac Centre, Al Amiri Hospital, Kuwait City, Kuwait.
- Department of Mathematics and Statistics, University of Strathclyde, Glasgow, UK.
- Department of Endemic and Infectious Diseases, Faculty of Medicine, Suez Canal University, Ismailia, Egypt.
- Division of Gastroenterology, Department of Medicine, Al Sabah Hospital, Shuwaikh Medical Area, Kuwait.
- Division of Gastroenterology, Department of Medicine, Jaber Al Ahmed Hospital, South Surra, Kuwait.
- Department of Medicine, Al Adan Hospital, Hadiya, Kuwait.
- Department of Medicine, Farwaniya Hospital, Farwaniya, Kuwait.
- Department of Medicine, Mubarak Al-Kabeer Hospital, Jabriya, Kuwait.
- Department of Obstetrics and Gynaecology, Maternity Hospital, Shuwaikh Medical Area, Kuwait.
- Department of Medicine, Al Amiri Hospital, Kuwait City, Kuwait.
- Department of Internal Medicine with the Subspecialty of Cardiology and Functional Diagnostics Named after V.S. Moiseev, Institute of Medicine, Peoples' Friendship University of Russia (RUDN University), Moscow, Russian Federation.
Abstract
Background: This study investigates in-hospital mortality amongst patients with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and its relation to serum levels of gamma-glutamyl transferase (GGT).
Methods: Patients were stratified according to serum levels of gamma-glutamyl transferase (GGT) (GGT<50 IU/L or GGT≥50 IU/L).
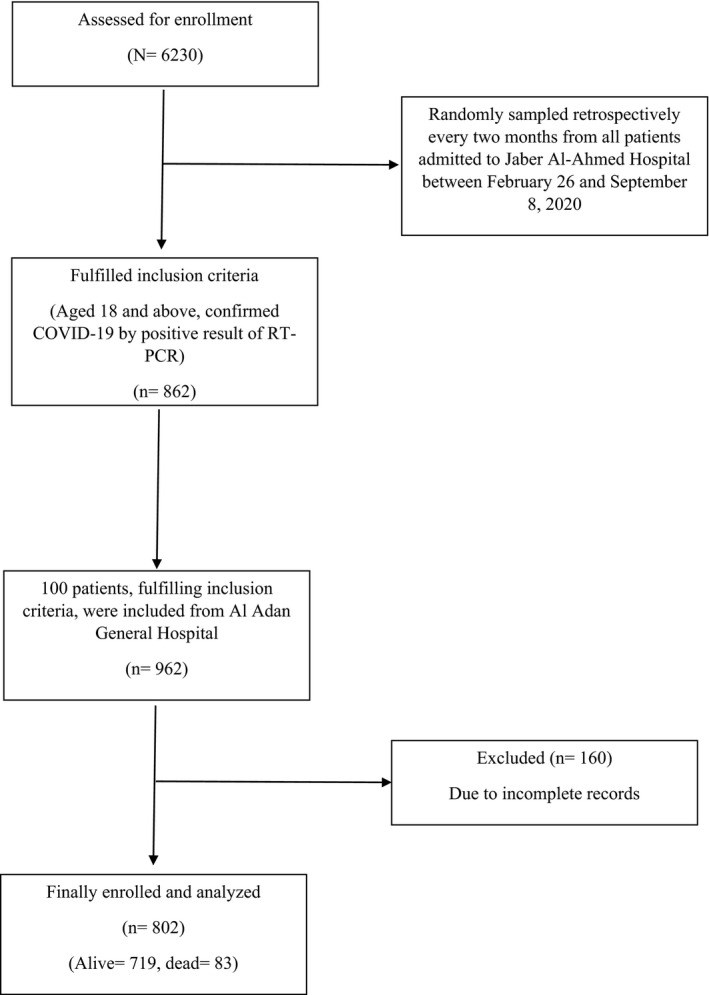
Results: A total of 802 participants were considered, amongst whom 486 had GGT<50 IU/L and a mean age of 48.1 (16.5) years, whilst 316 had GGT≥50 IU/L and a mean age of 53.8 (14.7) years. The chief sources of SARS-CoV-2 transmission were contact (366, 45.7%) and community (320, 40%). Most patients with GGT≥50 IU/L had either pneumonia (247, 78.2%) or acute respiratory distress syndrome (ARDS) (85, 26.9%), whilst those with GGT<50 IU/L had hypertension (141, 29%) or diabetes mellitus (DM) (147, 30.2%). Mortality was higher amongst patients with GGT≥50 IU/L (54, 17.1%) than amongst those with GGT<50 IU/L (29, 5.9%). More patients with GGT≥50 required high (83, 27.6%) or low (104, 34.6%) levels of oxygen, whereas most of those with GGT<50 had no requirement of oxygen (306, 71.2%). Multivariable logistic regression analysis indicated that GGT≥50 IU/L (odds ratio [OR]: 2.02, 95% confidence interval [CI]: 1.20-3.45, p=0.009), age (OR: 1.05, 95% CI: 1.03-1.07, p<0.001), hypertension (OR: 2.06, 95% CI: 1.19-3.63, p=0.011), methylprednisolone (OR: 2.96, 95% CI: 1.74-5.01, p<0.001) and fever (OR: 2.03, 95% CI: 1.15-3.68, p=0.016) were significant predictors of all-cause cumulative mortality. A Cox proportional hazards regression model (B = -0.68, SE =0.24, HR =0.51, p = 0.004) showed that patients with GGT<50 IU/L had a 0.51-times lower risk of all-cause cumulative mortality than patients with GGT≥50 IU/L.
Conclusion: Higher levels of serum GGT were found to be an independent predictor of in-hospital mortality.
Keywords: COVID-19; SARS-CoV-2; gamma-glutamyl transferase; in-hospital mortality.
Conflict of interest statement
No conflict of interest to disclose for any author on this manuscript.
Figures
Similar articles
Caravaca-Fontán F, Azevedo L, Bayo MÁ, Gonzales-Candia B, Luna E, Caravaca F.Nefrologia. 2017 May-Jun;37(3):267-275. doi: 10.1016/j.nefro.2016.11.010.PMID: 28648203 English, Spanish.
Aksakal E, Tanboga IH, Kurt M, Kaygın MA, Kaya A, Isik T, Ekinci M, Sevimli S, Acikel M.Atherosclerosis. 2012 Apr;221(2):596-601. doi: 10.1016/j.atherosclerosis.2012.01.044. Epub 2012 Feb 3.PMID: 22369933
Hartl L, Haslinger K, Angerer M, Jachs M, Simbrunner B, Bauer DJM, Semmler G, Scheiner B, Eigenbauer E, Strassl R, Breuer M, Kimberger O, Laxar D, Trauner M, Mandorfer M, Reiberger T.Liver Int. 2022 Jun;42(6):1297-1307. doi: 10.1111/liv.15274. Epub 2022 May 5.PMID: 35412018 Free PMC article.
Itabashi F, Hirata T, Kogure M, Narita A, Tsuchiya N, Nakamura T, Nakaya N, Sasaki R, Takanashi N, Sakata K, Tanno K, Sugawara J, Kuriyama S, Tsuji I, Kure S, Hozawa A.J Epidemiol. 2022 May 5;32(5):221-227. doi: 10.2188/jea.JE20200384. Epub 2021 Jun 22.PMID: 33390464 Free PMC article.
Zorlu A, Yucel H, Bektasoglu G, Turkdogan KA, Eryigit U, Sarikaya S, Ege MR, Tandogan I, Yilmaz MB.Am J Emerg Med. 2012 Jul;30(6):908-15. doi: 10.1016/j.ajem.2011.12.040. Epub 2012 Mar 3.PMID: 22386346
Cited by
In-hospital mortality in SARS-CoV-2 stratified by the use of corticosteroid.
Alotaibi N, Alroomi M, Aboelhassan W, Hussein S, Rajan R, AlNasrallah N, Al Saleh M, Ramadhan M, Zhanna KD, Pan J, Malhas H, Abdelnaby H, Almutairi F, Al-Bader B, Alsaber A, Abdullah M.Ann Med Surg (Lond). 2022 Aug;80:104105. doi: 10.1016/j.amsu.2022.104105. Epub 2022 Jun 29.PMID: 35784615 Free PMC article.
KMEL References
References
-
- Hanigan MH, Frierson HF Jr. Immunohistochemical detection of gamma‐glutamyl transpeptidase in normal human tissue. J Histochem Cytochem. 1996;44:1101‐1108. - PubMed
-
- Whitfield JB. Gamma glutamyl transferase. Crit Rev Clin Lab Sci. 2001;38:263‐355. - PubMed
-
- Saini N, Saini RK, Kumari M, et al. Evaluation of gamma glutamyl‐transferase (GGT) levels in COVID‐19: a retrospective analysis in tertiary care centre. Indian J Biochem Biophys. 2020;57(6):681‐686.
-
- Laine T, Reyes EM. Tutorial: survival estimation for Cox regression models with time‐varying coefficients using SAS and R. J Stat Softw. 2014;61:1‐23.
-
- Asghar MS, Akram M, Rasheed U, et al. Derangements of Liver enzymes in Covid‐19 positive patients of Pakistan: a retrospective comparative analysis with other populations. Archives of Microbiology & Immunology. 2020;4:110‐120.
-
- Daeppen JB, Smith TL, Schuckit MA. Influence of age and body mass index on gamma‐glutamyltransferase activity: a 15‐year follow‐up evaluation in a community sample. Alcohol Clin Exp Res. 1998;22:941‐944. - PubMed
-
- Tu W‐J, Liu Q, Cao J‐L, et al. γ‐Glutamyl transferase as a risk factor for all‐cause or cardiovascular disease mortality among 5912 ischemic strokes. Stroke. 2017;48(10):2888‐2891. - PubMed
![FIGURE 2 Kaplan–Meier survival plot of mortality according to GGT levels in patients with coronavirus disease [COVID‐19]. X‐axis: Days since admission](/Images/Figures/29_224.jpeg)