High Prevalence of New Delhi Metallo-β-Lactamase-1 (NDM-1) Producers among Carbapenem-Resistant Enterobacteriaceae in Kuwait
Affiliations
Affiliations
- Department of Microbiology, Faculty of Medicine, Kuwait University and Microbiology Unit, Mubarak Al Kabir Hospital, Jabriya, Kuwait.
Abstract
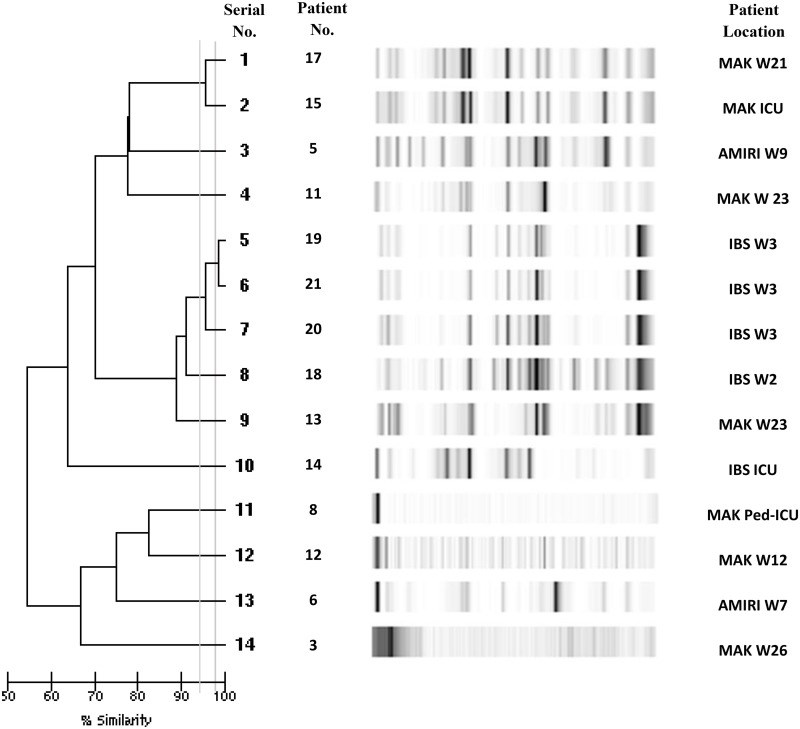
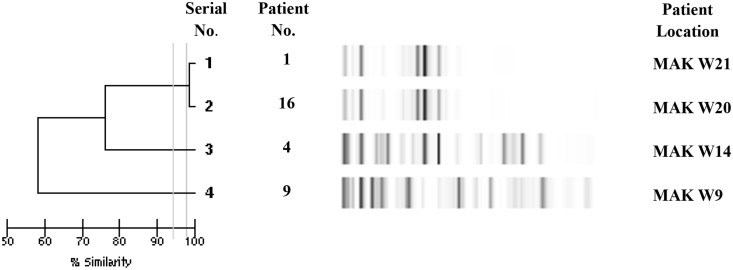
The aim of the study was to determine the prevalence of New Delhi metallo-β lactamase-1 (NDM-1) producing Enterobacteriaceae in Kuwait over a one year period. Consecutive Enterobacteriaceae isolates with reduced susceptibility to carbapenems were collected from four government hospitals in Kuwait from January-December 2014. Their susceptibility to 18 antibiotics was performed by determining the minimum inhibitory concentration. Isolates resistant to carbapenems were tested by PCR for resistant genes. Finger printing of the positive isolates was done by DiversiLab®. Clinical data of patients harboring NDM-1 positive isolates were analyzed. A total of 764 clinically significant Enterobacteriaceae isolates were studied. Of these, 61 (8%) were carbapenem-resistant. Twenty one out of these 61 (34.4%) were NDM-1-producers. All patients positive for NDM-1-carrying bacteria were hospitalized. About half were females (11/21 [52.3%]), average age was 53.3 years and the majority were Kuwaitis (14/21 [66.6%]). Six patients (28.5%) gave a history of travel or healthcare contact in an endemic area. Mortality rate was relatively high (28.6%). The predominant organism was Klebsiella pneumoniae (14 [66.6%]) followed by E. coli (4 [19%]). All NDM-1-positive isolates were resistant to meropenem, ertapenem, cefotaxime, cefoxitin and ampicillin, while 95.2% were resistant to imipenem, cefepime, and piperacillin-tazobactam. They were multidrug resistant including resistance to tigecycline, but 90% remained susceptible to colistin. About two-thirds of isolates (61.9%) co-produced-extended spectrum β-lactamases. During the study period, an outbreak of NDM-1 positive K. pneumoniae occurred in one hospital involving 3 patients confirmed by DiversiLab® analysis. In conclusion, NDM-1-producing Enterobacteriaceae is a growing healthcare problem with increasing prevalence in Kuwait, especially in hospitalized patients, leaving few therapeutic options. A high prevalence of NDM-1 necessitates the implementation of strict infection control to prevent the spread of these organisms.
Conflict of interest statement
Competing Interests: The authors have declared that no competing interest exist.
Figures
Similar articles
Jamal W, Rotimi VO, Albert MJ, Khodakhast F, Nordmann P, Poirel L.J Med Microbiol. 2013 Aug;62(Pt 8):1239-1244. doi: 10.1099/jmm.0.059915-0. Epub 2013 May 2.PMID: 23639985
Deshpande P, Rodrigues C, Shetty A, Kapadia F, Hedge A, Soman R.J Assoc Physicians India. 2010 Mar;58:147-9.PMID: 20848811
Huang YS, Tsai WC, Li JJ, Chen PY, Wang JT, Chen YT, Chen FJ, Lauderdale TL, Chang SC.Sci Rep. 2021 Jan 28;11(1):2609. doi: 10.1038/s41598-021-82166-8.PMID: 33510280 Free PMC article.
Bushnell G, Mitrani-Gold F, Mundy LM.Int J Infect Dis. 2013 May;17(5):e325-33. doi: 10.1016/j.ijid.2012.11.025. Epub 2013 Jan 16.PMID: 23332300 Review.
Charan J, Mulla S, Ryavanki S, Kantharia N.Pan Afr Med J. 2012;11:22. Epub 2012 Feb 13.PMID: 22514756 Free PMC article. Review.
Cited by
Al Fadhli AH, Mouftah SF, Jamal WY, Rotimi VO, Ghazawi A.Antibiotics (Basel). 2023 Jun 21;12(7):1081. doi: 10.3390/antibiotics12071081.PMID: 37508177 Free PMC article.
Alemayehu E, Fiseha T, Gedefie A, Alemayehu Tesfaye N, Ebrahim H, Ebrahim E, Fiseha M, Bisetegn H, Mohammed O, Tilahun M, Gebretsadik D, Debash H, Gobezie MY.BMC Infect Dis. 2023 May 3;23(1):277. doi: 10.1186/s12879-023-08237-5.PMID: 37138285 Free PMC article.
Al Dabbagh M, Alghounaim M, Almaghrabi RH, Dbaibo G, Ghatasheh G, Ibrahim HM, Aziz MA, Hassanien A, Mohamed N.Infect Dis Ther. 2023 May;12(5):1217-1235. doi: 10.1007/s40121-023-00799-w. Epub 2023 Apr 18.PMID: 37071349 Free PMC article. Review.
Tesfa T, Mitiku H, Edae M, Assefa N.Syst Rev. 2022 Nov 15;11(1):240. doi: 10.1186/s13643-022-02110-3.PMID: 36380387 Free PMC article.
Shahid M, Ahmad N, Saeed NK, Shadab M, Joji RM, Al-Mahmeed A, Bindayna KM, Tabbara KS, Dar FK.Front Cell Infect Microbiol. 2022 Oct 11;12:1033305. doi: 10.3389/fcimb.2022.1033305. eCollection 2022.PMID: 36304935 Free PMC article.
KMEL References
References
-
- Centers for Disease Control and Prevention (CDC). Antibiotic resistance threats in the United States. Atlanta, GA, USA: 2013. Available: http://www.cdc.gov/drugresistance/threat-report-2013/.
-
- Yong D, Toleman MA, Giske CG, Cho HS, Sundman K, Lee K, et al. Characterization of a new metallo-β-lactamase-1 gene, blaNDM-1, and a novel erythromycin esterase gene carried on a unique genetic structure in Klebsiella pneumoniae sequence type 14 from India. Antimicrob Agents Chemother. 2009; 53: 5046–5054. 10.1128/AAC.00774-09 - DOI - PMC - PubMed
-
- Al Sweih N, Jamal W, Rotimi VO. Spectrum and antibiotic resistance of uropathogens isolated from hospital and community patients with urinary tract infections in two large hospitals in Kuwait. Med Princ Pract. 2005; 14: 401–407. - PubMed
-
- Jamal W, Rotimi VO, Albert MJ, Khodakhast F, Udo EE, Poirel L. Emergence of nosocomial New Delhi metallo-β-lactamase-1 (NDM-1)-producing Klebsiella pneumoniae in patients admitted to a tertiary care hospital in Kuwait. Int J Antimicrob Agents. 2012; 39: 183–184. 10.1016/j.ijantimicag.2011.10.002 - DOI - PubMed
-
- Clinical and Laboratory Standards Institute (CLSI). Performance Standards for Antimicrobial susceptibility testing; Twenty Fourth Informational Supplement M100-S24. Wayne, Philadelphia; 2014.
-
- Zowawi HM, Sartor AL, Balkhy HH, Walsh TR, Al Johani SM, AlJindan RY, et al. Molecular characterization of carbapenemase-producing Escherichia coli and Klebsiella pneumoniae in the countries of the Gulf Cooperation Council: dominance of OXA-48 and NDM producers. Antimicrob Agents Chemother. 2014; 58: 3085–3090. 10.1128/AAC.02050-13 - DOI - PMC - PubMed
-
- Baroud M, Dandache I, Araj GF, Wakim R, Kanji S, Kanafani Z, et al. Underlying mechanisms of carbapenem resistance in extended-spectrum β-lactamase-producing Klebsiella pneumoniae and Escherichia coli isolates at a tertiary care centre in Lebanon: role of OXA-48 and NDM-1 carbapenemases. Int J Antimicrob Agents. 2013; 41: 75–79. 10.1016/j.ijantimicag.2012.08.010 - DOI - PubMed
-
- Kumarasamy KK, Toleman MA, Walsh TR, Bagaria J, Butt F, Balakrishnan R, et al. Emergence of a new antibiotic resistance mechanism in India, Pakistan, and the UK: a molecular, biological, and epidemiological study. Lancet Infect Dis. 2010; 10: 597–602. 10.1016/S1473-3099(10)70143-2 - DOI - PMC - PubMed
-
- Struelens MJ, Monnet DL, Magiorakos AP, Santos O’Connor F, Giesecke J, the European NDM-1 survey participants. New Delhi metallo-β-lactamase 1-producing Enterobacteriaceae: emergence and response in Europe. Euro Surveill. 2010; 15 Available: http://www.eurosurveillance.org/ViewArticle.aspx?articleld=19716. - PubMed
-
- Garcia-Fernandez A, Miriagou V, Papagiannitsis, Giordano A, Venditti M, Mancini C, et al. An ertapenem-resistant extended-spectrum-β-lactamase-producing Klebsiella pneumoniae clone carries a novel OmpK36 porin variant. Antimicrob Agents Chemother. 2010; 54: 4178–4184. 10.1128/AAC.01301-09 - DOI - PMC - PubMed
-
- Hidalgo L, Hopkins KL, Gutierrez B, Ovejero CM, Shukla S, Douthwaite S, et al. Association of the novel aminoglycoside resistance determinant RmtF with NDM carbapenemase in Enterobacteriaceae isolated in India and the UK. J Antimicrob Chemother. 2013; 68: 1543–1550. 10.1093/jac/dkt078 - DOI - PubMed
-
- Centers for Disease Control and Prevention (CDC). Facility guidance for control of carbapenem-resistant Enterobacteriaceae (CRE). November 2015 update- CRE toolkit. Available: http://www.cdc.gov/hai/pdfs/cre/CRE-guidance-508/.