Candida lusitaniae in Kuwait: Prevalence, antifungal susceptibility and role in neonatal fungemia
Affiliations
Affiliations
- Department of Microbiology, Faculty of Medicine, Kuwait University, Safat, Kuwait.
- Microbiology Department, Maternity Hospital, Shuwaikh, Kuwait.
Abstract
Objectives: Candida lusitaniae is an opportunistic yeast pathogen in certain high-risk patient populations/cohorts. The species exhibits an unusual antifungal susceptibility profile with tendency to acquire rapid resistance. Here, we describe prevalence of C. lusitaniae in clinical specimens in Kuwait, its antifungal susceptibility profile and role in neonatal fungemia.
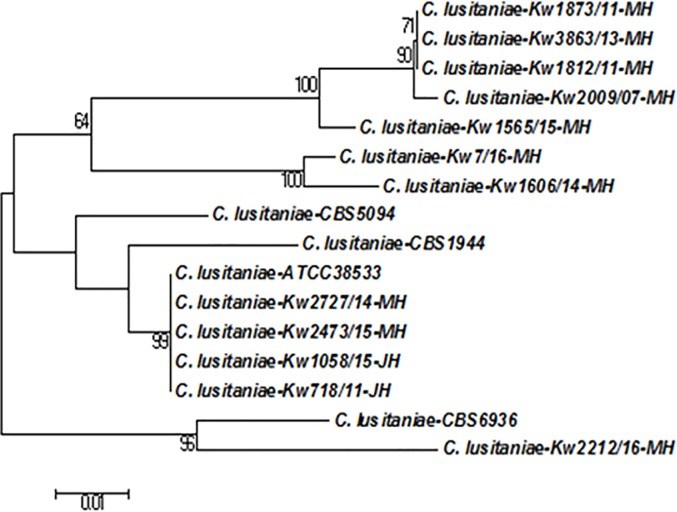
Methods: Clinical C. lusitaniae isolates recovered from diverse specimens during 2011 to 2017 were retrospectively analyzed. All isolates were identified by germ tube test, growth on CHROMagar Candida and by Vitek 2 yeast identification system. A simple species-specific PCR assay was developed and results were confirmed by PCR-sequencing of ITS region of rDNA. Antifungal susceptibility was determined by Etest. Minimum inhibitory concentrations (MICs) were recorded after 24 h incubation at 35°C.
Results: Of 7068 yeast isolates, 134 (1.89%) were identified as C. lusitaniae including 25 (2.52%) among 990 bloodstream isolates. Species-specific PCR and PCR-sequencing of rDNA confirmed identification. Of 11 cases of neonatal candidemia, 9 occurred in NICU of Hospital A and are described here. Eight of 9 neonates received liposomal amphotericin B, which was followed by fluconazole in 7 and additionally by caspofungin in 2 cases as salvage therapy. Three of 8 (37.5%) patients died. No isolate exhibited reduced susceptibility to amphotericin B, fluconazole, voriconazole, caspopfungin, micafungin and anidulafungin. The MIC ± geometric mean values for amphotericin B, fluconazole, voriconazole, and caspofungin were as follows: 0.072 ± 0.037 μg/ml, 2.32 ± 0.49 μg/ml, 0.09 ± 0.01 μg/ml and 0.16 ± 0.08 μg/ml, respectively. Only two isolates exhibited reduced susceptibility to fluconazole.
Conclusions: This study describes the prevalence and antifungal susceptibility profile of clinical C. lusitaniae isolates in Kuwait. No isolate showed reduced susceptibility to amphotericin B. The study highlights the emerging role of C. lusitaniae as a healthcare-associated pathogen capable of causing fungemia in preterm neonates and causing significant mortality.
Conflict of interest statement
The authors have declared that no competing interests exist.
Figures
Similar articles
Khan Z, Ahmad S, Al-Sweih N, Joseph L, Alfouzan W, Asadzadeh M.PLoS One. 2018 Apr 9;13(4):e0195743. doi: 10.1371/journal.pone.0195743. eCollection 2018.PMID: 29630658 Free PMC article.
Candida and candidaemia. Susceptibility and epidemiology.
Arendrup MC.Dan Med J. 2013 Nov;60(11):B4698.PMID: 24192246 Review.
Ahmad S, Khan Z, Al-Sweih N, Alfouzan W, Joseph L.Mycoses. 2020 Jan;63(1):104-112. doi: 10.1111/myc.13022. Epub 2019 Nov 3.PMID: 31618799
Candida kefyr in Kuwait: Prevalence, antifungal drug susceptibility and genotypic heterogeneity.
Ahmad S, Khan Z, Al-Sweih N, Alfouzan W, Joseph L, Asadzadeh M.PLoS One. 2020 Oct 27;15(10):e0240426. doi: 10.1371/journal.pone.0240426. eCollection 2020.PMID: 33108361 Free PMC article.
Arastehfar A, Daneshnia F, Salehi MR, Zarrinfar H, Khodavaisy S, Haas PJ, Roudbary M, Najafzadeh MJ, Zomorodian K, Charsizadeh A, Brouwer C, Pan W, Hagen F, Boekhout T.J Med Microbiol. 2019 May;68(5):770-777. doi: 10.1099/jmm.0.000963. Epub 2019 Mar 29.PMID: 30924763 Review.
Cited by
An Unconventional Oral Candidiasis in an Immunocompetent Patient.
Fusco A, Contaldo M, Savio V, Baroni A, Ferraro GA, Di Stasio D, Lucchese A, Chiaromonte A, Donnarumma G, Serpico R.J Fungi (Basel). 2023 Feb 24;9(3):295. doi: 10.3390/jof9030295.PMID: 36983463 Free PMC article.
Overview on the Infections Related to Rare Candida Species.
Kumar S, Kumar A, Roudbary M, Mohammadi R, Černáková L, Rodrigues CF.Pathogens. 2022 Aug 24;11(9):963. doi: 10.3390/pathogens11090963.PMID: 36145394 Free PMC article. Review.
Fatal Lodderomyces elongisporus Fungemia in a Premature, Extremely Low-Birth-Weight Neonate.
Asadzadeh M, Al-Sweih N, Ahmad S, Khan S, Alfouzan W, Joseph L.J Fungi (Basel). 2022 Aug 26;8(9):906. doi: 10.3390/jof8090906.PMID: 36135631 Free PMC article.
Candida lusitaniae: Biology, Pathogenicity, Virulence Factors, Diagnosis, and Treatment.
Mendoza-Reyes DF, Gómez-Gaviria M, Mora-Montes HM.Infect Drug Resist. 2022 Aug 31;15:5121-5135. doi: 10.2147/IDR.S383785. eCollection 2022.PMID: 36068831 Free PMC article. Review.
Al-Obaid I, Asadzadeh M, Ahmad S, Alobaid K, Alfouzan W, Bafna R, Emara M, Joseph L.J Fungi (Basel). 2022 Mar 6;8(3):267. doi: 10.3390/jof8030267.PMID: 35330269 Free PMC article.
KMEL References
References
-
- van Uden N, Buckley H. Candida Berkhout p. 893–1087. In Lodder J. (ed.). The yeasts. A taxonomic study. North-Holland Publishing Co; Amsterdam: 1970.
-
- Wingard JR. Importance of Candida species other than C. albicans as pathogens in oncology patients. Clin Infect Dis. 1995; 20: 115–125. - PubMed
-
- Clancy C, Nguyen M, Yu V. Fungemia caused by Candida lusitaniae Infections in medicine, 1996; 13: 940, 948–951.
-
- Jamal WY, Ahmad S, Khan ZU, Rotimi VO. Comparative evaluation of two matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS) systems for the identification of clinically significant yeasts. Int J Infect Dis. 2014; 26:167–170. 10.1016/j.ijid.2014.05.031 - DOI - PubMed
-
- Asadzadeh M, Ahmad S, Hagen F, Meis JF, Al-Sweih N, Khan Z. Simple, low-cost detection of Candida parapsilosis complex isolates and molecular fingerprinting of Candida orthopsilosis strains in Kuwait by ITS region sequencing and amplified fragment length polymorphism analysis. PLoS One 2015; 10: e0142880 10.1371/journal.pone.0142880 - DOI - PMC - PubMed
-
- Khan ZU, Ahmad S, Mokaddas E, Chandy R, Cano J, Guarro J. Actinomucor elegans var. kuwaitiensis isolated from the wound of a diabetic patient. Antonie van Leeuwoenhoek 2008; 94: 343–352. - PubMed
-
- Khan ZU, Ahmad S, Hagen F, Fell JW, Kowshik T, Chandy R, Boekhout T. Cryptococcus randhawai sp. nov., a novel anamorphic basidiomycetous yeast isolated from tree trunk hollow of Ficus religiosa (peepal tree) from New Delhi, India. Antonie Van Leeuwenhoek 2010; 97: 253–259. 10.1007/s10482-009-9406-8 - DOI - PubMed
-
- Ahmad S, Khan Z, Mustafa AS, Khan ZU. Epidemiology of Candida colonization in an intensive care unit of a teaching hospital in Kuwait. Med Mycol 2003; 41: 487–493. - PubMed
-
- Hadfield TL, Smith MB, Winn RE, Rinaldi MG, Guerra C. Mycoses caused by Candida lusitaniae. Rev Infect Dis. 1987; 9:1006–12. - PubMed
-
- Fowler SL, Rhoton B, Springer SC, Messer SA, Hollis RJ, Pfaller MA. Evidence for person-to-person transmission of Candida lusitaniae in a neonatal intensive-care unit. Infect Control Hosp Epidemiol. 1998; 19:343–5. - PubMed
-
- Pfaller MA, Andes DR, Diekema DJ, Horn DL, Reboli AC, Rotstein C., et al. Epidemiology and outcomes of invasive candidiasis due to non-albicans species of Candida in 2,496 patients: data from the Prospective Antifungal Therapy (PATH) registry 2004–2008. PLoS One. 2014; 9: e101510 10.1371/journal.pone.0101510 - DOI - PMC - PubMed
-
- Nguyen MH, Morris AJ, Dobson ME, Yu VL. Candida lusitaniae: An important emerging cause of candidemia. Infect Dis Clini Pract. 1996,5:273–278.
-
- Diekema DJ, Messer SA, Boyken LB, Hollis RJ, Kroeger J, Tendolkar S, et al. In vitro activity of seven systemically active antifungal agents against a large global collection of rare Candida species as determined by CLSI broth microdilution methods. J Clin Microbiol. 2009; 47: 3170–3177. 10.1128/JCM.00942-09 - DOI - PMC - PubMed
-
- Faria-Ramos I, Neves-Maia J, Ricardo E, Santos-Antunes J, Silva AT, Costa-de-Oliveira S, et al. Species distribution and in vitro antifungal susceptibility profiles of yeast isolates from invasive infections during a Portuguese multicenter survey. Eur J Clin Microbiol Infect Dis. 2014; 33: 2241–2247. 10.1007/s10096-014-2194-8 - DOI - PubMed
-
- Montagna MT, Lovero G, Borghi E, Amato G, Andreoni S, Campion L, et al. Candidemia in intensive care unit: a nationwide prospective observational survey (GISIA-3 study) and review of the European literature from 2000 through 2013. Eur Rev Med Pharmacol Sci. 2014; 18: 661–674. - PubMed
-
- Orasch C, Marchetti O., Garbino J., Schrenzel J., Zimmerli S., Muhlethaler K., et al. Candida species distribution and antifungal susceptibility testing according to European Committee on Antimicrobial Susceptibility Testing and new vs. old Clinical and Laboratory Standards Institute clinical breakpoints: a 6-year prospective candidaemia survey from the fungal infection network of Switzerland. Clin Microbiol Infect. 2014; 20: 698–705 10.1111/1469-0691.12440 - DOI - PubMed
-
- Chorro-Mari V, Christiansen N. Safety of high dose micafungin for the treatrment of fungal infections in neonates. Abstracts from the Neonatal and Paediatric Pharmacists Group (NPPG) 20th Annual Meeting (P. 13). Arch Dis Child. 2015; 100: e1.
-
- Christenson JC, Guruswamy A, Mukwaya G, Rettig PJ. Candida lusitaniae: an emerging human pathogen. Pediatr Infect Dis J. 1987; 6:755–757. - PubMed
-
- François F, Noël T, Pépin R, Brulfert A, Chastin C, Favel A, et al. Alternative identification test relying upon sexual reproductive abilities of Candida lusitaniae strains isolated from hospitalized patients. J Clin Microbiol. 2001; 39: 3906–3914. 10.1128/JCM.39.11.3906-3914.2001 - DOI - PMC - PubMed
-
- Favel A, Michel-Nguyen A, Peyron F, Martin C, Thomachot L, Datry A, et al. Colony morphology switching of Candida lusitaniae and acquisition of multidrug resistance during treatment of a renal infection in a newborn: case report and review of the literature. Diagn Microbiol Infect Dis. 2003; 47:331–339. - PubMed
-
- Pfaller MA, Espinel-Ingroff A, Bustamante B, Canton E, Diekema DJ, Fothergill A, et al. Multicenter study of anidulafungin and micafungin MIC distributions and epidemiological cutoff values for eight Candida species and the CLSI M27-A3 broth microdilution method. Antimicrob Agents Chemother. 2014; 58:916–922. 10.1128/AAC.02020-13 - DOI - PMC - PubMed
-
- Sanchez PJ, Cooper BH. Candida lusitaniae: sepsis and meningitis in a neonate. Pediatr Infect Dis J. 1987; 6:758–759. - PubMed
-
- Yinnon AM, Woodin KA, Powell KR. Candida lusitaniae infection in the newborn: case report and review of the literature. Pediatr Infect Dis J. 1992; 11: 878–880. - PubMed
-
- Levy O, Bourquin JP, McQueen A, Cantor AB, Lachenauer C, Malley R. Fatal disseminated Candida lusitaniae infection in an infant with chronic granulomatous disease. Pediatr Infect Dis J. 2002; 21:262–264. - PubMed
-
- Gautam MK, Li J. Neonatal Candida lusitaniae Septicemia. J Nepal Paediatr Soc 2014; 34: 160–162.
-
- Sariguzel FM, Koc AN, Ozturk M. Candida Utilis and Candida lusitaniae Meningitis in an infant with extraventricular drainage. Van Tıp Derg 2017; 24: 40–43.