Microbiological profile of diabetic foot ulcers in Kuwait
Affiliations
Affiliations
- Medical Division, Dasman Diabetes Institute, Kuwait City, Kuwait.
- Biochemistry & Molecular Biology Department, Research Division, Dasman Diabetes Institute, Kuwait City, Kuwait.
Abstract
Introduction: Diabetic foot ulcers (DFU) and infection (DFI) are a major diabetes-related problem around the world due to the high prevalence of diabetes in the population. The aim of our study was to determine the microbiological profile of infected ulcers in patients attending Dasman Diabetes Institute (DDI) clinics in Kuwait and to analyze the distribution of microbial isolates according to wound grade, sex, age and diabetes control.
Methods: We collected and analyzed clinical data and samples from 513 diabetic patients with foot ulcers referred to our podiatry clinic at DDI from Jan 2011 till Dec 2017.
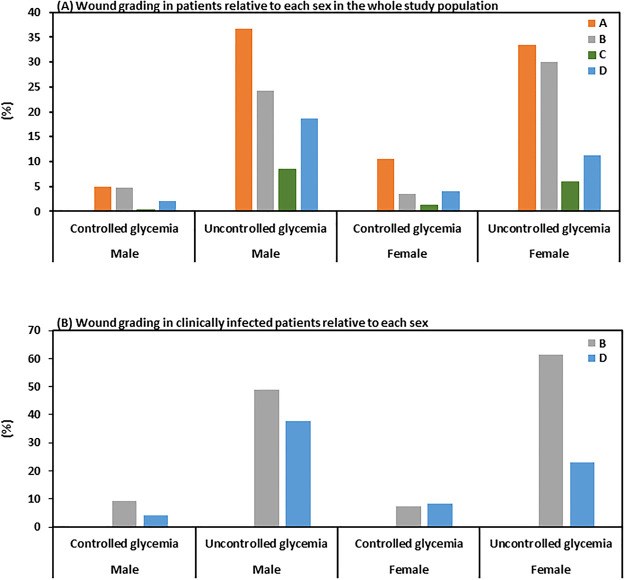
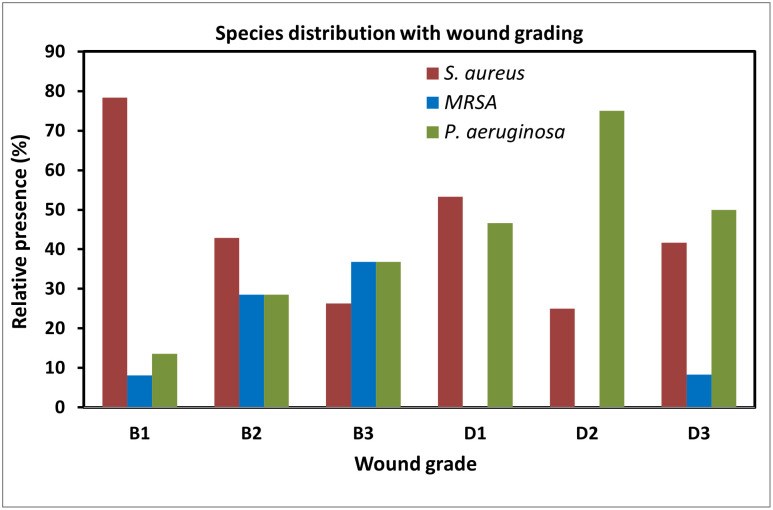
Results: We show a higher prevalence of DFU in men than in women, and a greater percentage of DFU occurred in men at an earlier age (p<0.05). Only about half of the DFU were clinically infected (49.3%) but 92% of DFU showed bacterial growth in the microbiological lab analysis. In addition, we isolated more monomicrobial (57.3%) than polymicrobial (34.8%) DFI and representing an average of 1.30 pathogens per patient. The presence of Gram-positive and Gram-negative strains was comparable between men and women regardless their age or glucose levels. Interestingly, more Gram-positive strains are present in ulcers without ischemia while more Gram-negative strains are present in ulcers with ischemia (p<0.05). While Staphylococcus aureus was common in infected ulcers without ischemia, Pseudomonas aeruginosa was predominant in ulcers with infection and ischemia, regardless of ulcer depth. Finally, a higher percentage of women has controlled HbA1c levels (19.41% versus 11.95% in men) and more women in this group displayed non-infected wounds (60.6% and 43.90% for women and men, respectively).
Conclusion: Our results provide an updated picture of the DFI patterns and antibiotics resistance in patients attending Dasman Diabetes Institute (DDI) clinics in Kuwait which might help in adopting the appropriate treatment of infected foot and improving clinical outcomes.
Conflict of interest statement
The authors have declared that no competing interests exist.
Figures
Similar articles
Nelson A, Wright-Hughes A, Backhouse MR, Lipsky BA, Nixon J, Bhogal MS, Reynolds C, Brown S; CODIFI collaborators.BMJ Open. 2018 Jan 31;8(1):e019437. doi: 10.1136/bmjopen-2017-019437.PMID: 29391370 Free PMC article.
Pattern and microbiological characteristics of diabetic foot ulcers in a Nigerian tertiary hospital.
Anyim O, Okafor C, Young E, Obumneme-Anyim I, Nwatu C.Afr Health Sci. 2019 Mar;19(1):1617-1627. doi: 10.4314/ahs.v19i1.37.PMID: 31148991 Free PMC article.
Microbiological profile and antimicrobial resistance among diabetic foot infections in Lebanon.
Jouhar L, Jaafar RF, Nasreddine R, Itani O, Haddad F, Rizk N, Hoballah JJ.Int Wound J. 2020 Dec;17(6):1764-1773. doi: 10.1111/iwj.13465. Epub 2020 Aug 11.PMID: 32779355 Free PMC article.
Du F, Ma J, Gong H, Bista R, Zha P, Ren Y, Gao Y, Chen D, Ran X, Wang C.Front Endocrinol (Lausanne). 2022 May 19;13:881659. doi: 10.3389/fendo.2022.881659. eCollection 2022.PMID: 35663325 Free PMC article. Review.
Shahrokh S, Aliye T, Yazdi M, Siavash M, Aminorroaya A.Int J Low Extrem Wounds. 2022 Dec;21(4):364-373. doi: 10.1177/15347346211002715. Epub 2021 Apr 28.PMID: 33909495 Review.
Cited by
Relative Abundance and Detection of Pseudomonas aeruginosa from Chronic Wound Infections Globally.
Phan S, Feng CH, Huang R, Lee ZX, Moua Y, Phung OJ, Lenhard JR.Microorganisms. 2023 May 5;11(5):1210. doi: 10.3390/microorganisms11051210.PMID: 37317184 Free PMC article. Review.
Classification Model for Diabetic Foot, Necrotizing Fasciitis, and Osteomyelitis.
Kim J, Yoo G, Lee T, Kim JH, Seo DM, Kim J.Biology (Basel). 2022 Sep 3;11(9):1310. doi: 10.3390/biology11091310.PMID: 36138789 Free PMC article.
Baig MS, Banu A, Zehravi M, Rana R, Burle SS, Khan SL, Islam F, Siddiqui FA, Massoud EES, Rahman MH, Cavalu S.Life (Basel). 2022 Jul 14;12(7):1054. doi: 10.3390/life12071054.PMID: 35888142 Free PMC article. Review.
Quazi A, Patwekar M, Patwekar F, Mezni A, Ahmad I, Islam F.Evid Based Complement Alternat Med. 2022 Jun 6;2022:1372199. doi: 10.1155/2022/1372199. eCollection 2022.PMID: 35707477 Free PMC article.
Xiong Y, Wu Q, Qin X, Yang C, Luo S, He J, Cheng Q, Wu Z.Front Vet Sci. 2022 Apr 21;9:850684. doi: 10.3389/fvets.2022.850684. eCollection 2022.PMID: 35529836 Free PMC article.
KMEL References
References
-
- Reiber GE, Smith DG, Carter J, Fotieo G, Deery HG 2nd, Sangeorzan JA, et al.: A comparison of diabetic foot ulcer patients managed in VHA and non-VHA settings. J Rehabil Res Dev 2001, 38:309–317. - PubMed
-
- Lavery LA, Armstrong DG, Wunderlich RP, Tredwell J, Boulton AJ: Diabetic foot syndrome: evaluating the prevalence and incidence of foot pathology in Mexican Americans and non-Hispanic whites from a diabetes disease management cohort. Diabetes Care 2003, 26:1435–1438. 10.2337/diacare.26.5.1435 - DOI - PubMed
-
- Epicast: EpiCast Report: Diabetic Foot Ulcers—Epidemiology Forecast to 2025. pp. 1–59; 2017:1–59.
-
- IDF: IDF Diabetes Atlas. vol. 9th edition pp. 1–176: International Diabetes Federation; 2019:1–176.
-
- Prompers L, Huijberts M, Apelqvist J, Jude E, Piaggesi A, Bakker K, et al.: High prevalence of ischaemia, infection and serious comorbidity in patients with diabetic foot disease in Europe. Baseline results from the Eurodiale study. Diabetologia 2007, 50:18–25. 10.1007/s00125-006-0491-1 - DOI - PubMed
-
- Sugandhi P, Prasanth DA: Bacteriological Profile of Diabetic Foot. International Journal of Innovative Research in Science 2014, 3:14688–14692.
-
- Levine NS, Lindberg RB, Mason AD Jr., Pruitt BA Jr.: The quantitative swab culture and smear: A quick, simple method for determining the number of viable aerobic bacteria on open wounds. J Trauma 1976, 16:89–94. - PubMed
-
- Bauer AW, Kirby WM, Sherris JC, Turck M: Antibiotic susceptibility testing by a standardized single disk method. Am J Clin Pathol 1966, 45:493–496. - PubMed
-
- Patil S, Mane R: Bacterial and clinical profile of diabetic foot ulcer using optimal culture techniques. International Journal of Research in Medical Sciences 2017, 5:496–502.
-
- Tascini C, Piaggesi A, Tagliaferri E, Iacopi E, Fondelli S, Tedeschi A, et al.: Microbiology at first visit of moderate-to-severe diabetic foot infection with antimicrobial activity and a survey of quinolone monotherapy. Diabetes Res Clin Pract 2011, 94:133–139. 10.1016/j.diabres.2011.07.017 - DOI - PubMed
-
- Rahim F, Ullah F, Ishfaq M, Afridi AK, Rahman SU, Rahman H: Frequency Of Common Bacteria And Their Antibiotic Sensitivity Pattern In Diabetics Presenting With Foot Ulcer. J Ayub Med Coll Abbottabad 2016, 28:528–533. - PubMed
-
- Xie X, Bao Y, Ni L, Liu D, Niu S, Lin H, et al.: Bacterial Profile and Antibiotic Resistance in Patients with Diabetic Foot Ulcer in Guangzhou, Southern China: Focus on the Differences among Different Wagner’s Grades, IDSA/IWGDF Grades, and Ulcer Types. Int J Endocrinol 2017, 2017:8694903 10.1155/2017/8694903 - DOI - PMC - PubMed
-
- EARSS: European Antimicrobial Resistance Surveillance System. The Netherlands; 2007.
-
- Kinross P, Petersen A, Skov R, Van Hauwermeiren E, Pantosti A, Laurent F, et al.: Livestock-associated meticillin-resistant Staphylococcus aureus (MRSA) among human MRSA isolates, European Union/European Economic Area countries, 2013. Euro Surveill 2017, 22 10.2807/1560-7917.ES.2017.22.44.16-00696 - DOI - PMC - PubMed