Dysmenorrhea among high-school students and its associated factors in Kuwait
Affiliations
Affiliations
- Department of Community Medicine and Behavioural Sciences, Faculty of Medicine, Kuwait University, Box: 24923, 13110, Safat, Kuwait.
- Department of Community Medicine and Behavioural Sciences, Faculty of Medicine, Kuwait University, Box: 24923, 13110, Safat, Kuwait. altaiar@hsc.edu.kw.
Abstract
Background: Although dysmenorrhea is not a life-threatening condition, it can cause a substantial burden on individuals and communities. There is no data on the prevalence of dysmenorrhea in Kuwait. This study aimed to estimate the prevalence of dysmenorrhea among female public high-school students in Kuwait and investigate factors associated with dysmenorrhea.
Methods: A cross-sectional study using multistage cluster sampling with probability proportional to size method was conducted on 763 twelfth grade female public high-school students (aged 16-21 years). We used face-to-face interview with a structured questionnaire to collect data on dysmenorrhea and presumed risk factors. Weight and height of the students were measured using appropriate weight and height scales in a standardized manner. The association between dysmenorrhea and potential risk factors was assessed using multiple logistic regression.
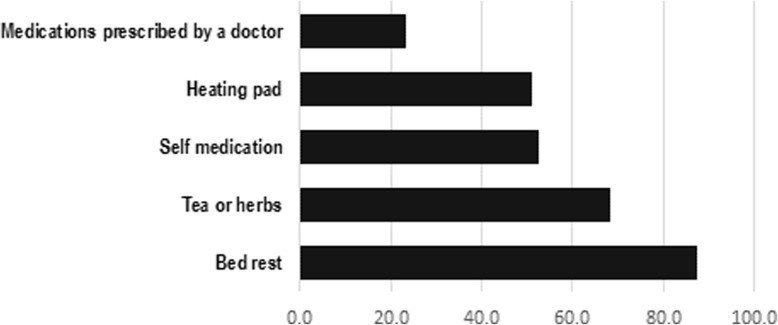
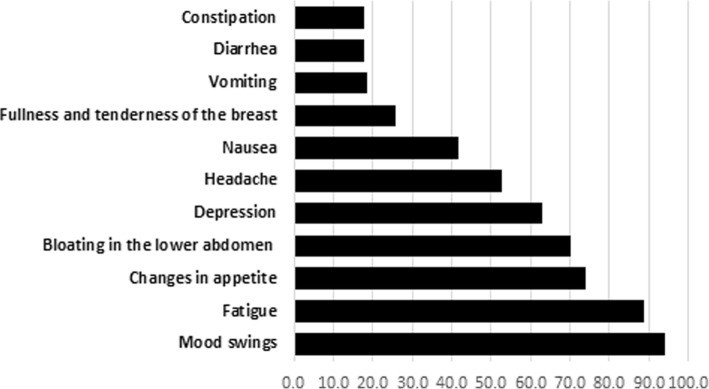
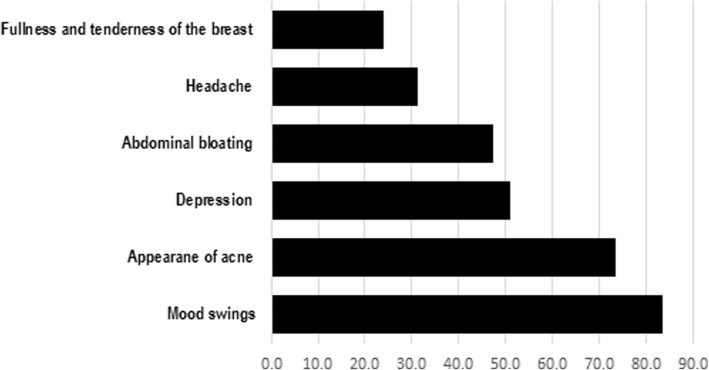
Results: The one-year prevalence of dysmenorrhea was found to be 85.6% (95%CI: 83.1-88.1%). Of the participants with dysmenorrhea, 26% visited a public or a private clinic for their pain and 4.1% were hospitalized for their menstrual pain. Furthermore, 58.2% of students with dysmenorrhea missed at least one school day and 13.9% missed at least one exam. Age of menarche (p-value = 0.005), regularity and flow of the menstrual period (p-value = 0.025, p-value = 0.009; respectively), and drinking coffee (p-value = 0.004) were significantly associated with dysmenorrhea in multivariable analysis.
Conclusion: Dysmenorrhea seems to be highly prevalent among female high-school students in Kuwait, resembling that of high-income countries. Because of the scale of the problem, utilizing school nurses to reassure and manage students with primary dysmenorrhea and referring suspected cases of secondary dysmenorrhea is recommended.
Keywords: Dysmenorrhea; Kuwait; Menstrual pain; School girls.
Conflict of interest statement
Ethics approval and consent to participate
The study was approved by The Ethics Committee at Health Science Center, Kuwait University (Ref: 3660–16/10/2017). Written informed consent was taken from each participant. As per the waiver from The Ethics Committee, no consents were sought from the parents.
Consent for publication
Not applicable as no individual data are published.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Figures
Similar articles
Hu Z, Tang L, Chen L, Kaminga AC, Xu H.J Pediatr Adolesc Gynecol. 2020 Feb;33(1):15-22. doi: 10.1016/j.jpag.2019.09.004. Epub 2019 Sep 17.PMID: 31539615
Muluneh AA, Nigussie TS, Gebreslasie KZ, Anteneh KT, Kassa ZY.BMC Womens Health. 2018 Apr 24;18(1):57. doi: 10.1186/s12905-018-0552-x.PMID: 29699536 Free PMC article.
Menstrual Cycle and Headache in Teenagers.
Bianchin L, Bozzola M, Battistella Pier A, Bernasconi S, Bona G, Buzi F, De Sanctis C, De Sanctis V, Tonini G, Radetti G, Rigon F, Perissinotto E.Indian J Pediatr. 2019 Jan;86(Suppl 1):25-33. doi: 10.1007/s12098-018-2829-3. Epub 2019 Jan 12.PMID: 30637681
De Sanctis V, Rigon F, Bernasconi S, Bianchin L, Bona G, Bozzola M, Buzi F, De Sanctis C, Tonini G, Radetti G, Perissinotto E.Indian J Pediatr. 2019 Jan;86(Suppl 1):34-41. doi: 10.1007/s12098-018-2822-x. Epub 2019 Jan 10.PMID: 30628040 Review.
Primary Dysmenorrhea in Adolescents: Prevalence, Impact and Recent Knowledge.
De Sanctis V, Soliman A, Bernasconi S, Bianchin L, Bona G, Bozzola M, Buzi F, De Sanctis C, Tonini G, Rigon F, Perissinotto E.Pediatr Endocrinol Rev. 2015 Dec;13(2):512-20.PMID: 26841639 Review.
Cited by
Ghandour R, Hammoudeh W, Stigum H, Giacaman R, Fjeld H, Holmboe-Ottesen G.Arch Public Health. 2023 Mar 30;81(1):47. doi: 10.1186/s13690-023-01059-6.PMID: 36998019 Free PMC article.
Mitsuhashi R, Sawai A, Kiyohara K, Shiraki H, Nakata Y.Int J Environ Res Public Health. 2022 Dec 29;20(1):569. doi: 10.3390/ijerph20010569.PMID: 36612891 Free PMC article. Review.
Huang WC, Chiu PC, Ho CH.J Sports Sci Med. 2022 Dec 1;21(4):595-607. doi: 10.52082/jssm.2022.595. eCollection 2022 Dec.PMID: 36523895 Free PMC article. Clinical Trial.
Mammo M, Alemayehu M, Ambaw G.Int J Womens Health. 2022 Nov 9;14:1569-1577. doi: 10.2147/IJWH.S384275. eCollection 2022.PMID: 36387327 Free PMC article.
Mesele TT, Ayalew HG, Syoum AT, Antehneh TA.Front Reprod Health. 2022 Jul 6;4:939035. doi: 10.3389/frph.2022.939035. eCollection 2022.PMID: 36303653 Free PMC article.
KMEL References
References
-
- Lobo RA, Gershenson DM, Lentz GM, Valea FA. Comprehensive gynecology E-book: Elsevier Health Sciences; 2016.
-
- Raine-Fenning N. Dysmenorrhoea. Curr Obstet Gynaecol. 2005;15(6):394–401. doi: 10.1016/j.curobgyn.2005.09.007. - DOI
-
- De Sanctis V, Soliman AT, Elsedfy H, Soliman NA, Soliman R, El Kholy M. Dysmenorrhea in adolescents and young adults: a review in different country. Acta Biomed. 2017;87(3):233–246. - PubMed
-
- Jones AE. Managing the pain of primary and secondary dysmenorrhoea. Nurs Times. 2004;100(10):40–43. - PubMed
-
- At a glance: Kuwait [https://www.unicef.org/infobycountry/kuwait_statistics.html#120].
-
- Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: visual analog scale for pain (VAS pain), numeric rating scale for pain (NRS pain), McGill pain questionnaire (MPQ), short-form McGill pain questionnaire (SF-MPQ), chronic pain grade scale (CPGS), short Form-36 bodily pain scale (SF-36 BPS), and measure of intermittent and constant osteoarthritis pain (ICOAP) Arthritis Care Res (Hoboken) 2011;63(S11):S240–S252. doi: 10.1002/acr.20543. - DOI - PubMed
-
- Ghaderi F, Asghari Jafarabadi M, Mohseni Bandpei MA. Dysmenorrhea and self-care strategies in Iranian female students: a regression modeling of pain severity and underlying factors. Int J Adolesc Med Health. 2016;29(6). - PubMed
-
- Subasinghe AK, Happo L, Jayasinghe YL, Garland SM, Gorelik A, Wark JD. Prevalence and severity of dysmenorrhoea, and management options reported by young Australian women. Aust Fam Physician. 2016;45(11):829–834. - PubMed
-
- French L. Dysmenorrhea. Am Fam Physician. 2005;71(2):285–91. - PubMed
-
- Alia S, Shamssain M, Shahwan M. Prevalence and impact of dysmenorrhea on health related quality of life in the United Arab Emirates. Eur J Pharm Med Res. 2016;3(2):77–86.
-
- Jensen D, Andersen K, Wagner G. Prostaglandins in the menstrual cycle of women. A review. Dan Med Bull. 1987;34(3):178–182. - PubMed
-
- Unsal A, Tozun M, Aslan G, Ayranci U, Alkan G. Evaluation of dysmenorrhea among women and its impact on quality of life in a region of western Turkey. Pak J Med Sci. 2010;26(1):142–147.
-
- Pejcic A, Jankovic S. Risk factors for dysmenorrhea among young adult female university students. Ann Ist Super Sanita. 2016;52(1):98–103. - PubMed
-
- Wilson C, Emans J, Mansfield J, Podolsky C, Grace E. The relationships of calculated percent body fat, sports participation, age, and place of residence on menstrual patterns in healthy adolescent girls at an independent new England high school. J Adolesc Health Care. 1984;5(4):248–253. doi: 10.1016/S0197-0070(84)80126-6. - DOI - PubMed