Examination of sleep in relation to dietary and lifestyle behaviors during Ramadan: A multi-national study using structural equation modeling among 24,500 adults amid COVID-19
Moien A B Khan 1, Ahmed S BaHammam 2, Asma Amanatullah 3, Khaled Obaideen 4, Teresa Arora 5, Habiba Ali 1, Leila Cheikh Ismail 6, Dana N Abdelrahim 7, Mohammed Al-Houqani 8, Kholoud Allaham 9, Rand Abdalrazeq 10, Wahid Sharif Aloweiwi 11, Somayea Sultana Mim 12, Ammar Mektebi 13, Sohrab Amiri 14, Sahabi Kabir Sulaiman 15, Syed Fahad Javaid 16, Mohammad Delwer Hossain Hawlader 17, Fatimah Isma'il Tsiga-Ahmed 18, Iffat Elbarazi 19, Saskiyanto Manggabarani 20, Gamechu Atomsa Hunde 21, Sabrina Chelli 22, Mitra Sotoudeh 23, MoezAlIslam Ezzat Faris 6; Ramadan Intermittent Fasting Collaborators
Affiliations
Affiliations
- 1College of Medicine and Health Sciences, United Arab Emirates University, Al Ain, United Arab Emirates.
- 2Department of Internal Medicine, College of Medicine, King Saud University, Riyadh, Saudi Arabia.
- 3Knowledge and Research Support Services Department, University of Management and Technology, Lahore, Pakistan.
- 4Sustainable Energy and Power Systems Research Centre, RISE, University of Sharjah, Sharjah, United Arab Emirates.
- 5Department of Psychology, Zayed University, Abu Dhabi, United Arab Emirates.
- 6Department of Clinical Nutrition and Dietetics, College of Health Sciences, University of Sharjah, Sharjah, United Arab Emirates.
- 7Sharjah Institute for Medical and Health Sciences, University of Sharjah, Sharjah, United Arab Emirates.
- 8Internal Medicine College of Medicine and Health Sciences, United Arab Emirates University, Al Ain, United Arab Emirates.
- 9Department of Neurology, Rashid Hospital, Dubai Health Authority, Dubai, United Arab Emirates.
- 10Faculty of Medicine, Mansoura University, Mansoura, Egypt.
- 11School of Medicine, The University of Jordan, Amman, Jordan.
- 12Chattogram International Medical College and Hospital, Chattogram, Bangladesh.
- 13Faculty of Medicine, Kütahya Health Sciences University, Kütahya, Türkiye.
- 14Medicine, Quran and Hadith Research Center, Baqiyatallah University of Medical Sciences, Tehran, Iran.
- 15Department of Internal Medicine, Yobe State University Teaching Hospital, Damaturu, Nigeria.
- 16Department of Psychiatry and Behavioral Science, College of Medicine and Health Sciences, United Arab Emirates University, Al Ain, United Arab Emirates.
- 17Department of Public Health, North South University, Dhaka, Bangladesh.
- 18Department of Community Medicine, Bayero University, Kano, Nigeria.
- 19Institute of Public Health, College of Medicine and Health Sciences, United Arab Emirates University, Al Ain, United Arab Emirates.
- 20Department of Nutrition, Sekolah Tinggi Ilmu Kesehatan Pertamedika, Jakarta, Indonesia.
- 21Faculty of Health Sciences, School of Nursing, Institute of Health, Jimma University, Jimma, Ethiopia.
- 22Royal College of Surgeons in Ireland (Bahrain), Al Muharraq, Bahrain.
- 23Iranshahr University of Medical Sciences, Iranshahr, Iran.
- 24National Pirogov Memorial Medical University, Vinnytsia, Ukraine; Faculty of Medicine, Al Quds University, Jerusalem, Palestine; Faculty of Medicine, Helwan University, Cairo, Egypt; Al-Quds University, Bethlehem, Palestine; Faculty of Medicine, Mansoura University Behbbit, Samannoud, Egypt; Qatar University, Mesaieed, Qatar; Department of Family Medicine, College of Medicine and Health Sciences, United Arab Emirates University, Al Ain, United Arab Emirates; RCSI-UCD, Ayer Keroh, Malaysia; Iran Sports Medicine Research Center, Neuroscience Institute Sports Medicine Research Center, Neuroscience Institute Tehran University of Medical Sciences, Tehran, Iran; Kasr Alainy Faculty of medicine, Cairo, Egypt; Kütahya Univerity of Health Sciences, kütahya, Türkiye; Trinity College Dublin, Dublin, Ireland; University of Tunis El Manar, Medical School of Tunis, Military Hospital of Tunis, Tunis, Tunisia; Department Public Health, Universitas Aufa Royhan Di Kota Padangsidimpuan, Padangsidimpuan, Indonesia; Orenburg state Medical University, Orenburg, Russia; Services Institute of Medical Sciences, Services Hospital Lahore House officer Services Institute of Medical Science, Lahore, Paksitan; Lebanese university, Beirut, Lebanon; University of Aleppo, Aleppo, Syria; Chemistry department, American University of Beirut, Beirut, Lebanon; Department of Medicine, Vinnytsia National Medical University, Abuja, Nigeria; Dentistry Programme of Mulawarman University Kerayan, Mulawarman University, Samarinda, Indonesia; Dentistry Programme, Mulawarman University Medical Education, Samarinda, Indonesia; Jordan University of Science and Technology, Irbid, Jordan; Sbks Medical College, Ahmedabad, India; Public Health Asharej, Jawarneh MPH UAEU, Al Ain, United Arab Emirates; Faculty of Medicine, Dental Medicine and Pharmacy of Fez, Sidi Mohammed Ben Abdellah University, Fez, Morocco; College of Medicine, National University for Science and Technology, Seeb, Oman; Ambulatory Healthcare Services, Abu Dhabi, United Arab Emirates; Department of Family Medicine, College of Medicine and Health Sciences, United Arab Emirates University, Abu Dhabi, United Arab Emirates; Dubai Medical College, Dubai, United Arab Emirates; Dubai medical college, Dubai, United Arab Emirates; Ambulatory Healthcare Services, Abu Dhabi, United Arab Emirates; Department of Family Medicine, College of Medicine and Health Sciences, United Arab Emirates University, Abu Dhabi, United Arab Emirates; Department of Endocrinology Syria, Faculty of Medicine, Aleppo University Hospital, University of Aleppo, Aleppo, Syria; Department of surgery, Jaber alahmed hospital, Kuwait City, Kuwait; Spinghar Thoracic Surgery Kabul, Kabul, Afghanistan; College of Food and Agriculture, United Arab Emirates University, Dubai, United Arab Emirates; Alexandria faculty of medicine, General practitioner, Alexandria, Egypt; Department of Nutrition Science, Universitas Muhammadiyah Surakarta, Sukoharjo, Indonesia; Tanjungpura University, Pontianak, Indonesia; MidHudson Family Medicine residency, Institute for family Health Family Medicine, Centerville, United States; OnDokuz Mayis University, Samsun, Turkey; Faculty of Medical Sciences, Lebanese university, Beirut, Lebanon; An-Najah National University, Nablus, Palestine; University of Jordan, Amman, Jordan; Ondokuz Mayis University, Samsun, Turkey; MPH, North South University, Dhaka, Bangladesh; Aljabili Saglik Bilimleri Üniversitesi, Istanbul, Turkey; Monash University, Fawkner, Australia; Ain Shams General Hospital House, Khartoum, Sudan; Tripoli central hospital, Tripoli, Libya; Aleppo University Hospital, Aleppo, Syria; Faculté de Médecine et de Pharmacie de Rabat, Temara, Morocco; NGHA, KAMC, Riyadh, Saudi Arabia; Surgery department (Intern doctor), Princess Basma teaching hospital, Irbid, Jordan; University of Aleppo, Aleppo, Syria; Medical Facuilty, Paktia University, Kabul, Afghanistan; Student Research Committee, Iran Clinical Research Development Center of Imam Khomeini Hospital, Jiroft University of Medical Sciences, Jiroft, Iran; College of Medicine, Qatar University, Doha, Qatar; Faculté de Médecine, de Pharmacie et de Médecine Dentaire de Fès, Fez, Morocco; Kas al aini Clinic, Cairo, Egypt; Department of Physiology, Alzaiem Alazhari University, Khartoum, North Sudan; Department of Human Physiology, Alzaiem Alazhari University, Khartoum, North Sudan; Ministry of Health Internship, Khartoum, Sudan; Ministry of Health, Khartoum, Sudan; The Department of Statistics, The Islamia University of Bahawalpur, Bahawalpur, Pakistan; College of Medicine, Menoufia University, Al Minufiyah, Egypt; Psychology Department of Behavioral Science, Rehman College of Dentistry, Peshawar, Pakistan; CMHS Family Medicine, UAEU, Al Ain, United Arab Emirates; Healthcare Psychology, Abu Dhabi, United Arab Emirates; ICU department, Alexandria Main University Hospital, Alexandria, Egypt; Mosul medical collage, Mosul, Iraq; Ondokuz Mayis University, Samsun, Turkey; Emirates Health Services, Dubai, United Arab Emirates; Faculty of Medicine, Ain Shams University, Cairo, Egypt; Department of Nutrition, Pertamedika College of Health Sciences, Jakarta, Indonesia; School of Nursing and Midwifery, Tehran University of Medical Sciences, Tarbiat Modares University, Tehran, Iran; Shadan Institute of Medical Sciences and Research Centre, Peeramcheru, India; CMH Institute of Medical Sciences, Multan, Pakistan; Birat Medical College and Teaching Hospital Sukhrampur, Krishnanagar, Nepal; Kuwait University, Kuwait City, Kuwait; Jordan University of Science and Technology, Irbid, Jordan; Alexandria Faculty of Medicine, Alexandria, Egypt; College of Medicine, King Saud bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia; King Abdulaziz Medical City, Ministry National Guard Health Affairs, Riyadh, Saudi Arabia; King Abdullah International Medical Research Center, Riyadh, Saudi Arabia; Nangarhar Medical Faculty, Timergara, Pakistan; Khatam-Al-Nabieen University, Kabul, Afghanistan; University of Debrecen, Debrecen, Hungary; Faculté de médecine d'Alger, Algiers, Algeria; Sultan Qaboos University (Oman), Seeb, Oman; JSS Medical College, Mysore General Medicine, Kannur, India; Jimma University, Jimma, Ethiopia; DNB GEM Hospital General Medicine, Chennai, India; An-Najah National University, Bethlehem, Palestine; MWACP West African College of Physicians, Federal Neuropsychiatric Hospital, Maiduguri, Nigeria; MBBCh Dubai Medical College, Manama, Bahrain.
Collaborators
- Ramadan Intermittent Fasting Collaborators:
Abasi-Okot Akpan Udoyen 24, Abdelrhman Muwafaq Janem 24, Abdullah Taha Zayed 24, Adriana Johny Skafi 24, Ahmed Ashraf Elmoghazy 24, Ahmed Daniyal Nawaz 24, Ahmed Juma AlKaabi 24, Sabri Amalin Najiha Binti Mohd 24, Amir Human-Hoveidaeiv 24, Amir N Attia 24, Ammar Mektebi 24, Amna Mohammed Al Zadjali 24, Anis Riahi 24, Anto Jamma Hadi 24, Ashish Ramesh Dubey 24, Ayesha Iqbal 24, Ali Bachar Jalal El 24, Bakri Yahia Roumi Jamal 24, Baraa Moujahed Hajjar 24, Chika Chizitelu Madekwe 24, Cicih Bhakti Purnamasari 24, Cicih Bhakti Purnamasari 24, Dawlah Qasem Murshed Ahmed Saeed 24, Dhaval Maunishkumar Shah 24, Dima Ibrahim 24, Diyae Khadri 24, Eman Younis Al-Fahdi 24, Fatema Al Mazrouei 24, Fatema Al Mazrouei 24, Fatema Muneer Radhi 24, Fatema Yusuf Aljanabi 24, Fatima Al Sheriff Al Zaabi 24, Fatima Al Sheriff Al Zaabi 24, Fatima Alzhra Mohamed Hanifa 24, Fatma Mustafa Ridha 24, Fayaz Ahmad Momand 24, Fayeza Hasan 24, Filopater Mar Gerges 24, Firmansyah Firmansyah Firmansyah 24, Frederick Putra Wijaya 24, Hassan B Nagy 24, Hussam Kiwan 24, Ibrahim Khaled Salah El Din 24, Israa Hasan Hasan 24, Jehad Firas Samhouri 24, Kamil Sannah 24, Lamisa Rahman 24, M Munir 24, Malik Bendak 24, Maram Sirelkhatim Elsayed 24, Marwa Mohammed Morgom 24, Maya Shahadeh Alassadi 24, Meryem Gounni 24, Moath Ahmed Aldafas 24, Mohammad Mahmoud Jarrah 24, Mohammad Shahrour 24, Mohammad Elyas Wardak 24, Mohammad Pourfridoni 24, Mohammad Zulqurnain Haider 24, Mohammed Chakir 24, Mohammed Al-Rsheed Mostafa Omar Abueissa 24, Mohannad Abdalfdeeel Almahie Shaban 24, Mohannad Abdalfdeel Almahie Shaban 24, Monzir Musa Hamdan Mohammed 24, Mosab Salah Elmahi Ahmed 24, Muhammad Daniyal Khan 24, Muhammad Sameh Amer 24, Muttahid Shah 24, Nadirah Ghenimi Ghenimi 24, Nailah Mahmood 24, Nermeen Mohammed Afifi 24, Noran Omar Mahmood 24, Noura Ahmad Kanjo 24, Rahaf Ziad Abughosh 24, Ramy Rafaat Yassa 24, Rani Rahmasari Tanuwijaya M Gizi 24, Reza Heidari-Soureshjani 24, Romana Riyaz 24, Rutab Tareen 24, Sajjad Ahmed Khan 24, Sana Kalim Qureshi 24, Sara Mohammed Ahmed Musleh Al Badani 24, Sara Nazmy Ataallah 24, Saud Mohammed Alwatban 24, Saud Mohammed Alwatban 24, Saud Mohammed Alwatban 24, Sayed Mustafa Kamal 24, Shams Ul Haq Noori 24, Somto Judith Okafor 24, Tadjadit Lydia 24, Tariq Ali Al Habsi 24, Tejaswini Ashok 24, Tujuba Diribsa Benti 24, Waseem N Ahmed 24, Yazan William Giacaman 24, Yesiru Adeyemi Kareem 24, Zainab Sadeq AlRabeea 24
Abstract
Background: Of around 2 billion Muslims worldwide, approximately 1.5 billion observe Ramadan fasting (RF) month. Those that observe RF have diverse cultural, ethnic, social, and economic backgrounds and are distributed over a wide geographical area. Sleep is known to be significantly altered during the month of Ramadan, which has a profound impact on human health. Moreover, sleep is closely connected to dietary and lifestyle behaviors.
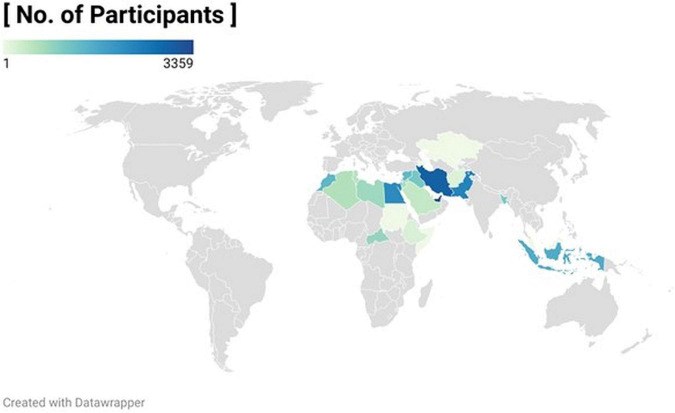
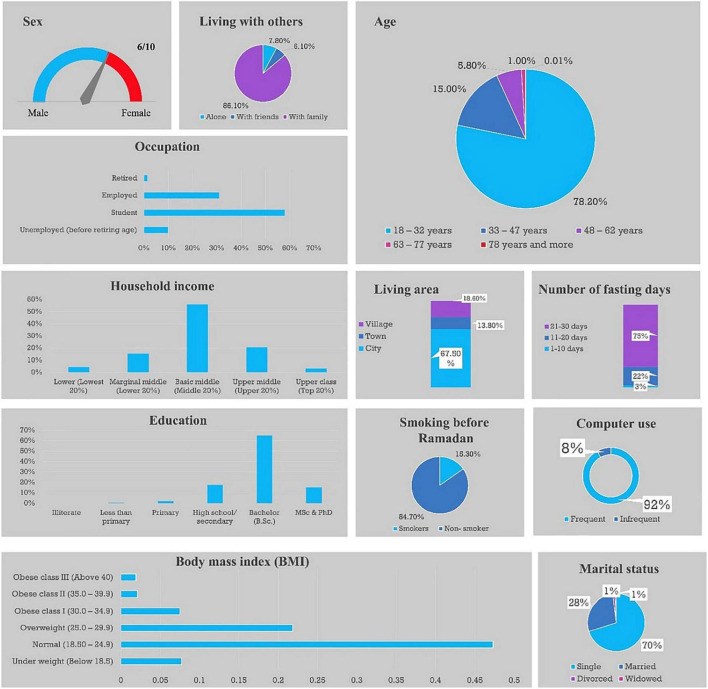
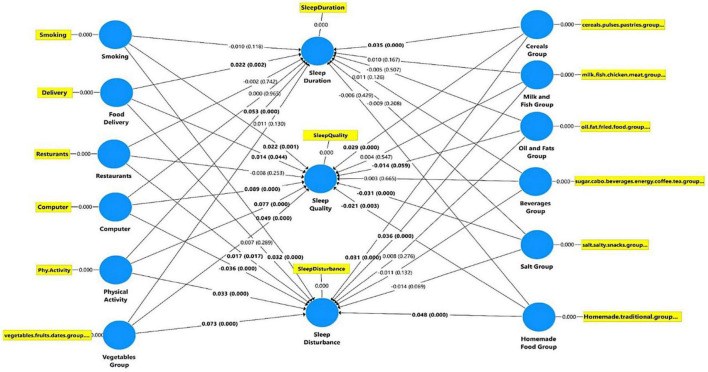
Methods: This cross-sectional study collected data using a structured, self-administered electronic questionnaire that was translated into 13 languages and disseminated to Muslim populations across 27 countries. The questionnaire assessed dietary and lifestyle factors as independent variables, and three sleep parameters (quality, duration, and disturbance) as dependent variables. We performed structural equation modeling (SEM) to examine how dietary and lifestyle factors affected these sleep parameters.
Results: In total, 24,541 adults were enrolled in this study. SEM analysis revealed that during RF, optimum sleep duration (7-9 h) was significantly associated with sufficient physical activity (PA) and consuming plant-based proteins. In addition, smoking was significantly associated with greater sleep disturbance and lower sleep quality. Participants that consumed vegetables, fruits, dates, and plant-based proteins reported better sleep quality. Infrequent consumption of delivered food and infrequent screen time were also associated with better sleep quality. Conflicting results were found regarding the impact of dining at home versus dining out on the three sleep parameters.
Conclusion: Increasing the intake of fruits, vegetables, and plant-based proteins are important factors that could help improve healthy sleep for those observing RF. In addition, regular PA and avoiding smoking may contribute to improving sleep during RF.
Keywords: Ramadan; diet; fasting; intermittent fasting; lifestyle and behavior; sleep.
Figures
Similar articles
Akbari HA, Yoosefi M, Pourabbas M, Weiss K, Knechtle B, Vancini RL, Trakada G, Ben Saad H, Lavie CJ, Ghram A.J Clin Med. 2022 Apr 22;11(9):2346. doi: 10.3390/jcm11092346.PMID: 35566470 Free PMC article.
Alzhrani A, Alhussain MH, BaHammam AS.Front Nutr. 2022 Sep 2;9:966861. doi: 10.3389/fnut.2022.966861. eCollection 2022.PMID: 36118763 Free PMC article.
Sulaiman SK, Tsiga-Ahmed FI, Faris ME, Musa MS, Akpan UA, Umar AM, Abubakar SM, Allaham KK, Alyammahi T, Abdbuljalil MA, Javaid SF, Khan MA.Int J Environ Res Public Health. 2022 Nov 2;19(21):14340. doi: 10.3390/ijerph192114340.PMID: 36361226 Free PMC article.
Ramadan intermittent fasting and immunity: An important topic in the era of COVID-19.
Faris MAE, Salem ML, Jahrami HA, Madkour MI, BaHammam AS.Ann Thorac Med. 2020 Jul-Sep;15(3):125-133. doi: 10.4103/atm.ATM_151_20. Epub 2020 Jun 18.PMID: 32831933 Free PMC article. Review.
Ramadan Fasting and NCDs-Example of the Diabetes.
Bencharif M, Sersar I, Bentaleb M, Boutata FZ, Benabbas Y.Front Nutr. 2022 Mar 2;9:787571. doi: 10.3389/fnut.2022.787571. eCollection 2022.PMID: 35308269 Free PMC article. Review.
KMEL References
References
-
- World Population Review. Muslim Population by Country. (2022). Available online at: https://worldpopulationreview.com/
-
- Abdelrahim D, Faris ME, Hassanein M, Shakir AZ, Yusuf AM, Almeneessier AS, et al. Impact of Ramadan diurnal intermittent fasting on hypoglycemic events in patients with type 2 diabetes: a systematic review of randomized controlled trials and observational studies. Front Endocrinol (Lausanne). (2021) 12:624423. 10.3389/fendo.2021.624423 - DOI - PMC - PubMed
-
- Faris M, Jahrami HA, Obaideen AA, Madkour MI. Impact of diurnal intermittent fasting during Ramadan on inflammatory and oxidative stress markers in healthy people: systematic review and meta-analysis. J Nutr Intermed Metab. (2019) 15:18–26. 10.1016/j.jnim.2018.11.005 - DOI
-
- Faris M, Jahrami H, BaHammam A, Kalaji Z, Madkour M, Hassanein M. A systematic review, meta-analysis, and meta-regression of the impact of diurnal intermittent fasting during Ramadan on glucometabolic markers in healthy subjects. Diabetes Res Clin Pract. (2020) 165:108226. - PubMed
-
- Al-Rawi N, Madkour M, Jahrami H, Salahat D, Alhasan F, BaHammam A, et al. Effect of diurnal intermittent fasting during Ramadan on ghrelin, leptin, melatonin, and cortisol levels among overweight and obese subjects: a prospective observational study. PLoS One. (2020) 15:e0237922. 10.1371/journal.pone.0237922 - DOI - PMC - PubMed
-
- Almeneessier AS, Bahammam AS, Sharif MM, Bahammam SA, Nashwan SZ, Perumal SRP, et al. The influence of intermittent fasting on the circadian pattern of melatonin while controlling for caloric intake, energy expenditure, light exposure, and sleep schedules: a preliminary report. Ann Thorac Med. (2017) 12:183. 10.4103/atm.ATM_15_17 - DOI - PMC - PubMed
-
- Jahrami H, BaHammam A, Kalaji Z, Madkour M, Hassanein M. A systematic review, meta-analysis, and meta-regression of the impact of diurnal intermittent fasting during Ramadan on glucometabolic markers in healthy subjects. Diabetes Res Clin Pract. (2020) 165:108226. - PubMed
-
- Almeneessier AS, Pandi-Perumal SR, BaHammam AS. Intermittent fasting, insufficient sleep, and circadian rhythm: interaction and effects on the cardiometabolic system. Curr Sleep Medicine Rep. (2018) 4:179–95. 10.1007/s40675-018-0124-5 - DOI
-
- Trabelsi K, Ammar A, Masmoudi L, Boukhris O, Chtourou H, Bouaziz B, et al. Sleep quality and physical activity as predictors of mental wellbeing variance in older adults during COVID-19 lockdown: ECLB COVID-19 international online survey. Int J Environ Res Public Health. (2021) 18:4329. 10.3390/ijerph18084329 - DOI - PMC - PubMed
-
- Ismail LC, Osaili TM, Mohamad MN, Al Marzouqi A, Jarrar AH, Zampelas A, et al. Assessment of eating habits and lifestyle during the coronavirus 2019 pandemic in the middle east and North Africa region: a cross-sectional study. Br J Nutr. (2021) 126:757–66. 10.1017/S0007114520004547 - DOI - PMC - PubMed
-
- World Medical Association. Declaration of Helsinki. Ethical principles for medical research involving human subjects. Jahrb Für Wiss Und Ethik. (2009) 14:233–8. 10.1515/9783110208856.233 - DOI
-
- Wild D, Grove A, Martin M, Eremenco S, McElroy S, Verjee-Lorenz A, et al. Principles of good practice for the translation and cultural adaptation process for patient-reported outcomes (PRO) measures: report of the ISPOR task force for translation and cultural adaptation. Value Health. (2005) 8:94–104. 10.1111/j.1524-4733.2005.04054.x - DOI - PubMed
-
- Masjedi MR, Ainy E, Zayeri F, Paydar R. Cigarette and hookah smoking in adolescent students using world health organization questionnaire global youth tobacco survey (GYTS): a pilot study in Varamin City, Iran in 2016. Asian Pac J Cancer Prev. (2020) 21:3033–7. 10.31557/APJCP.2020.21.10.3033 - DOI - PMC - PubMed
-
- World Health Organization. Global Youth Tobacco Survey (GYTS), Bhutan Report, 2013. Geneva: World Health Organization; (2015).
-
- Deschasaux-Tanguy M, Druesne-Pecollo N, Esseddik Y, De Edelenyi FS, Allès B, Andreeva VA, et al. Diet and physical activity during the coronavirus disease 2019 (COVID-19) lockdown (March–May 2020): results from the French nutrinet-santé cohort study. Am J Clin Nutr. (2021) 113:924–38. 10.1093/ajcn/nqaa336 - DOI - PMC - PubMed
-
- World Health Organization. Body Mass Index–BMI. Geneva: World Health Organization; (2022).
-
- Rose S. The growing Size and Incomes of the Upper Middle Class. (Vol. 21). Washington, DC: Urban Institute; (2016). p. 10
-
- Centers for Disease Control and Prevention Government Agency. Sleep and Sleep Disorders/How Much Sleep Do I Need?. Atlanta, GA: Centers for Disease Control and Prevention Government Agency; (2022).
-
- Fan Y, Chen J, Shirkey G, John R, Wu SR, Park H, et al. Applications of structural equation modeling (SEM) in ecological studies: an updated review. Ecol Processes. (2016) 5:19. 10.1186/s13717-016-0063-3 - DOI
-
- Ringle CM, Wende S, Becker JM. SmartPLS. Boenningstedt: SmartPLS GmbH; (2015).
-
- David Garson G. Partial Least Squares: Regression & Structural Equation Models. Raleigh, NC: Statistical Publishing Associates; (2016).
-
- Henseler J, Ringle CM, Sarstedt M. A new criterion for assessing discriminant validity in variance-based structural equation modeling. J Acad Mark Sci. (2015) 43:115–35. 10.1007/s11747-014-0403-8 - DOI
-
- Hair JF, Jr, Hult GTM, Ringle CM, Sarstedt M. A Primer on Partial Least Squares Structural Equation Modeling (PLS-SEM). Thousand Oaks, CA: Sage publications; (2021). 10.1007/978-3-030-80519-7 - DOI
-
- Min C, Kim H-J, Park I-S, Park B, Kim J-H, Sim S, et al. The association between sleep duration, sleep quality, and food consumption in adolescents: a cross-sectional study using the Korea youth risk behavior web-based survey. BMJ Open. (2018) 8:e022848. 10.1136/bmjopen-2018-022848 - DOI - PMC - PubMed
-
- Zuraikat FM, Makarem N, St-Onge M-P, Xi H, Akkapeddi A, Aggarwal B. A Mediterranean dietary pattern predicts better sleep quality in US women from the American heart association go red for women strategically focused research network. Nutrients. (2020) 12:2830. 10.3390/nu12092830 - DOI - PMC - PubMed
-
- Wang F, Boros S. The effect of physical activity on sleep quality: a systematic review. Eur J Physiother. (2021) 23:11–8. 10.1080/21679169.2019.1623314 - DOI
-
- Ammar K, Hermassi S, Kolahi A, Mansournia MA, Jahrami H, Boukhris O, et al. Global disease burden attributed to low physical activity in 204 countries and territories from 1990 to 2019: insights from the global burden of disease 2019 study. Biol Sport. (2023) 40:835–55. 10.5114/biolsport.2023.121322 - DOI
-
- Bollen KA, Pearl J. Eight myths about causality and structural equation models. In: Morgan SL. editor. Handbook of Causal Analysis for Social Research. (New York, NY: Springer; ) (2013). p. 301–28. 10.1007/978-94-007-6094-3_15 - DOI
-
- Washif J, Pyne DB, Sandbakk Ø, Trabelsi K, Aziz AR, Beaven C, et al. Ramadan intermittent fasting induced poorer training practices during the COVID-19 lockdown: a global cross-sectional study with 5529 athletes from 110 countries. Biol Sport. (2022) 39:1103–15. 10.5114/biolsport.2022.117576 - DOI - PMC - PubMed