Effectiveness of virtual mindfulness-based interventions on perceived anxiety and depression of physicians during the COVID-19 pandemic: A pre-post experimental study
Affiliations
Affiliations
- Faculty of Medicine, Kuwait University, Kuwait City, Kuwait.
- Amiri Hospital, Ministry of Health, Kuwait City, Kuwait.
- Dasman Diabetes Institute, Kuwait City, Kuwait.
- Centre for Mindfulness Research and Practice, Bangor University, Bangor, United Kingdom.
Abstract
Background: The outbreak of coronavirus disease 2019 (COVID-19) created unprecedented stress on physicians. Mindfulness is a type of meditation that focuses on being fully present, aware of senses, and emotions in the present moment without analyzing or judging them, and it may help reduce psychological distress in physicians. This study aimed to examine the effectiveness of virtual mindfulness-based intervention (MBI) on physicians' perceived anxiety and depression and different facets of mindfulness.
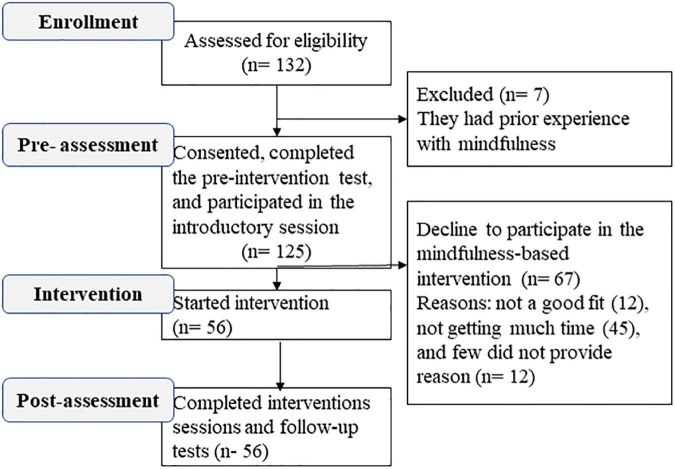
Methods: During the COVID-19 pandemic, an online survey was administered to physicians to assess depression, anxiety, and awareness using the 9-item Patient Health Questionnaire (PHQ-9), 7-item General Anxiety Disorder (GAD-7), and Five-Facets Mindfulness Questionnaire (FFMQ), respectively. Physicians that received the virtual MBI sessions also completed post-questionnaires at a 3-week follow-up time point.
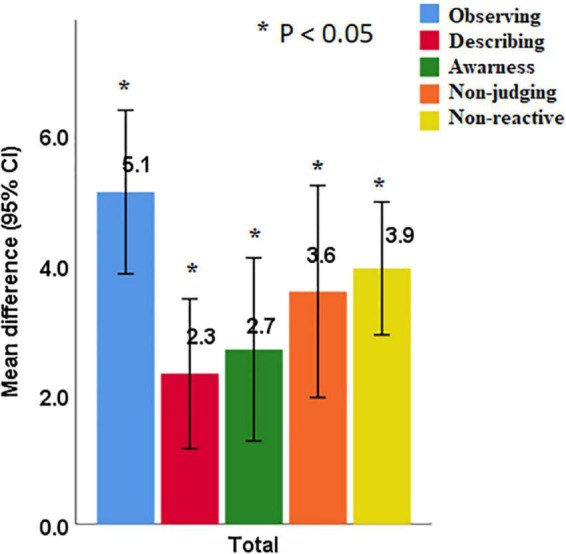
Results: A total of 125 physicians responded to the online survey, with 56 completing the MBI. The prevalence of moderate to severe anxiety and depression was 45.0 and 46.7%, respectively. Mindfulness scores were negatively associated with depression (r = -0.38, P < 0.001) and anxiety (r = -0.36, p < 0.001). Mindfulness scores for the 56 physicians who received virtual MBI sessions were significantly improved (mean difference ± SD, 17.7 ± 16.1, p = 0.001). Significant reductions were also evidenced in anxiety (4.4 ± 4.2) and depression (4.5 ± 5.1) scores (p's < 0.001). There was also an improvement in mindfulness facets of observing (5.1 ± 4.7), describing (2.3 ± 4.3), acting with awareness (2.7 ± 5.3), non-judging of inner experience (3.6 ± 6.1), and non-reactivity to inner experience (3.9 ± 4.0) (p's < 0.001). A facet of mindfulness, acting with awareness was most efficiently associated with improved anxiety (B = -0.3, p = 0.02) and depression (B = -0.4, p = 0.01).
Conclusion: This study has demonstrated that virtual MBI improved physicians' psychological wellbeing and mindfulness during the crisis. Regular mindfulness practice may help physicians to tolerate and handle unpleasant circumstances, such as future epidemics or pandemics.
Keywords: anxiety; depression; healthcare profession; mindfulness-based interventions (MBIs); physicians.
Conflict of interest statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Figures
Similar articles
Nissen ER, Zachariae R, O'Connor M, Kaldo V, Jørgensen CR, Højris I, Borre M, Mehlsen M.Internet Interv. 2021 Jan 14;23:100365. doi: 10.1016/j.invent.2021.100365. eCollection 2021 Mar.PMID: 33552930 Free PMC article.
El Morr C, Ritvo P, Ahmad F, Moineddin R; MVC Team.JMIR Ment Health. 2020 Jul 17;7(7):e18595. doi: 10.2196/18595.PMID: 32554380 Free PMC article.
Navarro-Haro MV, Modrego-Alarcón M, Hoffman HG, López-Montoyo A, Navarro-Gil M, Montero-Marin J, García-Palacios A, Borao L, García-Campayo J.Front Psychol. 2019 Jan 28;10:55. doi: 10.3389/fpsyg.2019.00055. eCollection 2019.PMID: 30745888 Free PMC article.
Querstret D, Cropley M, Fife-Schaw C.Mindfulness (N Y). 2018;9(6):1825-1836. doi: 10.1007/s12671-018-0925-0. Epub 2018 May 2.PMID: 30524514 Free PMC article.
Shi Z, MacBeth A.Mindfulness (N Y). 2017;8(4):823-847. doi: 10.1007/s12671-016-0673-y. Epub 2017 Jan 19.PMID: 28757900 Free PMC article. Review.
Cited by
Alsaeed D, Al-Ozairi A, Alsarraf H, Albarrak F, Al-Ozairi E.Front Public Health. 2023 Mar 30;11:1048283. doi: 10.3389/fpubh.2023.1048283. eCollection 2023.PMID: 37064685 Free PMC article.
Effect of COVID-19 vaccine on blood glucose metrics in Arabic people with type 1 diabetes.
Al-Ozairi E, Irshad M, Taghadom E, Varghese A, Sojan L, Alkandari J.Front Endocrinol (Lausanne). 2023 Mar 20;14:1120384. doi: 10.3389/fendo.2023.1120384. eCollection 2023.PMID: 37020598 Free PMC article.
Al-Ozairi A, Taghadom E, Irshad M, Al-Ozairi E.Diabetes Metab Syndr Obes. 2023 Feb 5;16:321-329. doi: 10.2147/DMSO.S377166. eCollection 2023.PMID: 36777315 Free PMC article.
KMEL References
References
-
- Allan S, Bealey R, Birch J, Cushing T, Parke S, Sergi G, et al. The prevalence of common and stress-related mental health disorders in healthcare workers based in pandemic-affected hospitals: a rapid systematic review and meta-analysis. Eur J Psychotraumatol. (2020) 11:1810903. 10.1080/20008198.2020.18109039 - DOI - PMC - PubMed
-
- Wang C, Pan R, Wan X, Tan Y, Xu L, Ho C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. (2020) 17:1729. 10.3390/ijerph170517299 - DOI - PMC - PubMed
-
- Marvaldi M, Mallet J, Dubertret C, Moro M, Guessoum S. Anxiety, depression, trauma-related, and sleep disorders among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Neurosci Biobehav Rev. (2021) 126:252–64. 10.1016/j.neubiorev.2021.03.0245 - DOI - PMC - PubMed
-
- Gilboa S, Shirom A, Fried Y, Cooper C. A meta-analysis of work demand stressors and job performance: examining main and moderating effects. Personnel Psychol. (2008) 61:227–71.
-
- Salari N, Khazaie H, Hosseinian-Far A, Khaledi-Paveh B, Kazeminia M, Mohammadi M, et al. The prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients: a systematic review and meta-regression. Hum Resour Health. (2020) 18:100. 10.1186/s12960-020-00544-1 - DOI - PMC - PubMed
-
- Gupta S, Kumar M, Rozatkar A, Basera D, Purwar S, Gautam D, et al. Feasibility and effectiveness of telecounseling on the psychological problems of frontline healthcare workers amidst COVID-19: a randomized controlled trial from Central India. Indian J Psychol Med. (2021) 43:343–50. 10.1177/025371762110245379 - DOI - PMC - PubMed
-
- Yıldırım D, Çiriş Yıldız C. The effect of mindfulness-based breathing and music therapy practice on nurses’ stress, work-related strain, and psychological well-being during the COVID-19 pandemic: a randomized controlled trial. Holist Nurs Pract. (2022) 36:156–65. 10.1097/HNP.00000000000005117 - DOI - PMC - PubMed
-
- McConville J, McAleer R, Hahne A. Mindfulness training for health profession students-the effect of mindfulness training on psychological well-being, learning and clinical performance of health professional students: a systematic review of randomized and non-randomized controlled trials. Explore. (2017) 13:26–45. 10.1016/j.explore.2016.10.0025 - DOI - PubMed
-
- Kabat-Zinn J. Mindfulness-based interventions in context: past, present, and future. Clin Psychol Sci Pract. (2003) 10:144–56. 10.1093/clipsy.bpg016 - DOI
-
- Chien W, Chow K, Chong Y, Bressington D, Choi K, Chan C. The role of five facets of mindfulness in a mindfulness-based psychoeducation intervention for people with recent-onset psychosis on mental and psychosocial health outcomes. Front Psychiatry. (2020) 11:177. 10.3389/fpsyt.2020.001777 - DOI - PMC - PubMed
-
- Spitzer R, Kroenke K, Williams J, Group P, Group P. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. JAMA. (1999) 282:1737–44. - PubMed
-
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. London: Routledge; (2013).
-
- Alsharji K. Anxiety and depression during the COVID-19 pandemic in Kuwait: the importance of physical activity. Middle East Curr Psychiatry. (2020) 27:60. 10.1186/s43045-020-00065-6 - DOI
-
- Magallón-Botaya R, Pérula-de Torres L, Verdes-Montenegro Atalaya J, Pérula-Jiménez C, Lietor-Villajos N, Bartolomé-Moreno C, et al. Mindfulness in primary care healthcare and teaching professionals and its relationship with stress at work: a multicentric cross-sectional study. BMC Fam Pract. (2021) 22:29. 10.1186/s12875-021-01375-29 - DOI - PMC - PubMed
-
- Gaspar I, Martinho A, Lima M. Exploring the benefits of a mindfulness program for Portuguese public healthcare workers. Curr Psychol. (2021) 40:772–81. 10.1007/s12144-018-9987-3 - DOI
-
- Alsubaie M, Abbott R, Dunn B, Dickens C, Keil T, Henley W, et al. Mechanisms of action in mindfulness-based cognitive therapy (MBCT) and mindfulness-based stress reduction (MBSR) in people with physical and/or psychological conditions: a systematic review. Clin Psychol Rev. (2017) 55:74–91. 10.1016/j.cpr.2017.04.0087 - DOI - PubMed
-
- Rodriguez-Vega B, Palao Á, Mu noz-Sanjose A, Torrijos M, Aguirre P, Fernández A, et al. Implementation of a mindfulness-based crisis intervention for frontline healthcare workers during the COVID-19 outbreak in a public general hospital in Madrid, Spain. Front Psychiatry. (2020) 11:562578. 10.3389/fpsyt.2020.562578 - DOI - PMC - PubMed
-
- Segal Z, Williams M, Teasdale J. Mindfulness-Based Cognitive Therapy for Depression. New York, NY: Guilford Publications; (2018).
-
- Royuela-Colomer E, Calvete E. Mindfulness facets and depression in adolescents: rumination as a mediator. Mindfulness. (2016) 7:1092–102. 10.1007/s12671-016-0547-3 - DOI
-
- Nolen-Hoeksema S, Wisco B, Lyubomirsky S. Rethinking rumination. Perspect Psychol Sci. (2008) 3:400–24. - PubMed