Cross-continental comparison of safety and protection measures amongst urologists during COVID-19
Jean de la Rosette 1, Pilar Laguna 1, Mario Álvarez-Maestro 2, Masatoshi Eto 3, Chaidir Arif Mochtar 4, Selami Albayrak 1, Arturo Mendoza-Valdes 5, Teng Aik Ong 6, Sanjay Khadgi 7, Abdullatif Al-Terki 8, Damien Bolton 9, Reynaldo Gomez 10, Laurence Klotz 11, Sanjay Kulkarni 12, Simon Tanguay 13, Stavros Gravas 14; Société Internationale d’Urologie Board of Directors
Affiliations
Affiliations
- Department of Urology, Faculty of Medicine, Istanbul Medipol University, Istanbul, Turkey.
- Department of Urology, La Paz University Hospital, Instituto de Investigación, Madrid, Spain.
- Department of Urology, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan.
- Department of Urology, Cipto Mangunkusumo Hospital, Faculty of Medicine, University of Indonesia, Jakarta, Indonesia.
- Department of Urology, Hospital Médica Sur, Mexico City, Mexico.
- Department of Surgery, Faculty of Medicine, University of Malaya, Kuala Lumpur, Malaysia.
- Department of Urology, Vayodha Hospitals, Kathmandu, Nepal.
- Urology Unit, Department of Surgery, Al-Amiri Hospital, Kuwait City, Kuwait.
- Department of Urology, The Austin Health, University of Melbourne, Melbourne, Victoria, Australia.
- Universidad Andrés Bello, Hospital del Trabajador, Santiago, Chile.
- Division of Urology, Sunnybrook Health Sciences Center, Toronto, Ontario, Canada.
- Kulkarni Reconstructive Urology Center, Pune, India.
- Division of Urology, Department of Surgery, McGill University, Montreal, Quebec, Canada.
- Department of Urology, Faculty of Medicine, School of Health Sciences, University of Thessaly, Larissa, Greece.
Abstract
Objectives: To determine the well-being of urologists worldwide during the coronavirus disease 2019 pandemic, and whether they have adequate personal protective equipment knowledge and supplies appropriate to their clinical setting.
Methods: Urologists worldwide completed a Société Internationale d'Urologie online survey from 16 April 2020 until 1 May 2020. Analysis was carried out to evaluate their knowledge about protecting themselves and others in the workplace, including their confidence in their ability to remain safe at work, and any regional differences.
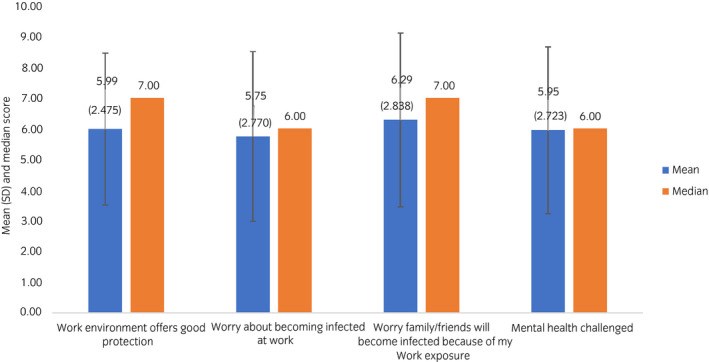
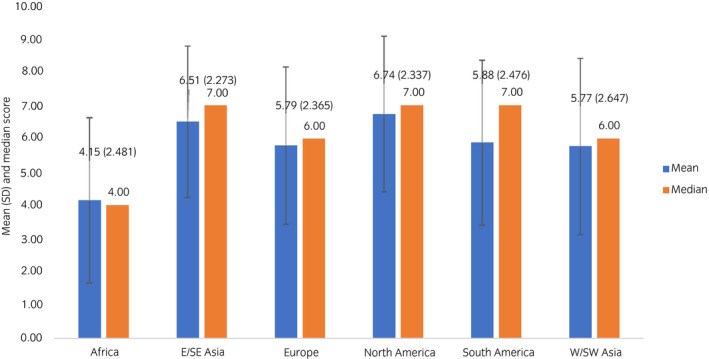
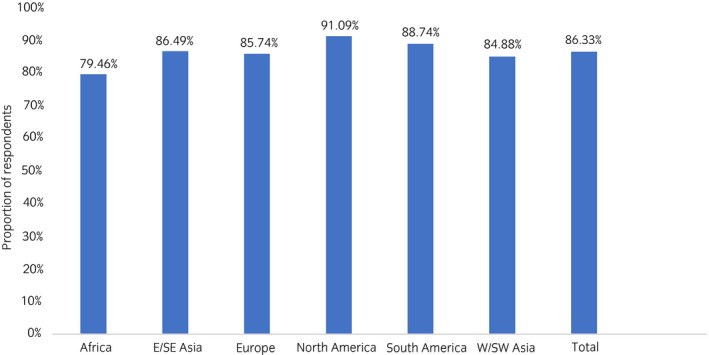
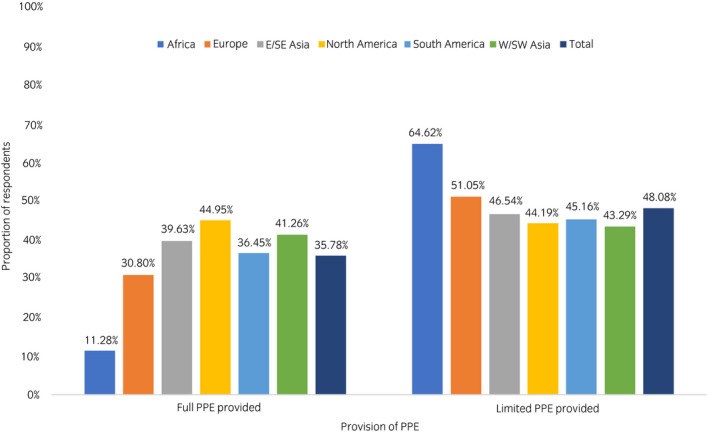
Results: There were 3488 respondents from 109 countries. Urologists who stated they were moderately comfortable that their work environment offers good protection against coronavirus disease 2019 showed a total mean satisfaction level of 5.99 (on a "0 = not at all" to "10 = very" scale). A large majority (86.33%) were confident about protecting themselves from coronavirus disease 2019 at work. However, only about one-third reported their institution provided the required personal protective equipment (35.78%), and nearly half indicated their hospital has or had limited personal protective equipment availability (48.08%). Worldwide, a large majority of respondents answered affirmatively for testing the healthcare team (83.09%). Approximately half of the respondents (52.85%) across all regions indicated that all surgical team members face an equal risk of contracting coronavirus disease 2019 (52.85%). Nearly one-third of respondents reported that they had experienced social avoidance (28.97%).
Conclusions: Our results show that urologists lack up-to-date knowledge of preferred protocols for personal protective equipment selection and use, social distancing, and coronavirus disease 2019 testing. These data can provide insights into functional domains from which other specialties could also benefit.
Keywords: COVID-19; pandemic; personal protective equipment; protective measures; urology.
Figures
Similar articles
Liu M, Cheng SZ, Xu KW, Yang Y, Zhu QT, Zhang H, Yang DY, Cheng SY, Xiao H, Wang JW, Yao HR, Cong YT, Zhou YQ, Peng S, Kuang M, Hou FF, Cheng KK, Xiao HP.BMJ. 2020 Jun 10;369:m2195. doi: 10.1136/bmj.m2195.PMID: 32522737 Free PMC article.
The Impact of the COVID-19 Pandemic on Urology Practice in Indonesia: A Nationwide Survey.
Rasyid N, Birowo P, Parikesit D, Rahman F.Urol J. 2020 Nov 4;17(6):677-679. doi: 10.22037/uj.v16i7.6459.PMID: 33159316
3D-printed protected face shields for health care workers in Covid-19 pandemic.
Lemarteleur V, Fouquet V, Le Goff S, Tapie L, Morenton P, Benoit A, Vennat E, Zamansky B, Guilbert T, Depil-Duval A, Gaultier AL, Tavitian B, Plaisance P, Tharaux PL, Ceccaldi PF, Attal JP, Dursun E.Am J Infect Control. 2021 Mar;49(3):389-391. doi: 10.1016/j.ajic.2020.08.005. Epub 2020 Aug 11.PMID: 32791260 Free PMC article.
COVID-19: Measures to prevent hospital contagion. What do urologists need to know?
Castro EIB, Secchi GL, Gómez CD, Gómez JT, Clark O, Alonso IAM, Salcedo JGC.Int Braz J Urol. 2020 Jul;46(suppl.1):113-119. doi: 10.1590/S1677-5538.IBJU.2020.S117.PMID: 32550704 Free PMC article. Review.
Hirschmann MT, Hart A, Henckel J, Sadoghi P, Seil R, Mouton C.Knee Surg Sports Traumatol Arthrosc. 2020 Jun;28(6):1690-1698. doi: 10.1007/s00167-020-06022-4. Epub 2020 Apr 27.PMID: 32342138 Free PMC article. Review.
Cited by
Quy Nguyen-Phuoc D, Ngoc Su D, Thanh Tran Dinh M, David Albert Newton J, Oviedo-Trespalacios O.Saf Sci. 2023 Jan;157:105920. doi: 10.1016/j.ssci.2022.105920. Epub 2022 Sep 6.PMID: 36091924 Free PMC article.
The impact the COVID-19 pandemic on urology literature: a bibliometric analysis.
Crocerossa F, Visser W, Carbonara U, Falagario UG, Pandolfo SD, Loizzo D, Imbimbo C, Klausner AP, Porpiglia F, Damiano R, Cantiello F, Autorino R.Cent European J Urol. 2022;75(1):102-109. doi: 10.5173/ceju.2021.291. Epub 2022 Jan 13.PMID: 35591965 Free PMC article. Review.
KMEL References
References
-
- Givi B, Schiff BA, Chinn SB et al. Recommendations for evaluation and surgery of the head and neck during the COVID‐19 pandemic. JAMA Otolaryngol. Head Neck Surg. 2020; 146: 579–84. - PubMed
-
- Murthy S, Gomersall CD, Fowler RA. Care for critically ill patients with COVID‐19. JAMA 2020; 323: 1499–500. - PubMed
-
- Sanders JM, Monogue MS, Jodlowski TZ, Cutrell JB. Pharmacologic treatments for coronavirus disease 2019 (COVID‐19): a review. JAMA 2020; 323: 1824–36. - PubMed
-
- Liang H, Archarya G. Novel corona virus disease (COVID‐19) in pregnancy: What clinical recommendations to follow? Acta Obstet. Gynecol. Scand. 2020; 99: 439–42. - PubMed
-
- MacIntyre CR, Dung TC, Seale H, Chughtai A. COVID‐19, shortages of masks and the use of cloth masks as a last resort. 2020. [Cited 5 Jun 2020.] Available from URL: https://bmjopen.bmj.com/content/5/4/e006577.responses#covid‐19‐shortages...
-
- Li Y, Wong T, Chung J et al. In vivo protective performance of N95 respirator and surgical facemasks. Am. J. Ind. Med. 2006; 49: 1056–65. - PubMed
-
- Desai AN, Aronoff DM Masks and Coronavirus Disease 2019 (COVID‐19). JAMA 2020; 323: 2103. - PubMed
-
- Grasselli G, Pesenti A, Cecconi M. Critical care utilization for the COVID‐19 outbreak in Lombardy, Italy: early experience and forecast during an emergency response. JAMA 2020; 323: 1545–6. - PubMed
-
- Hopman J, Allegranzi B, Mehtar S. Managing COVID‐19 in low‐ and middle‐income countries. JAMA 2020; 323: 1549–50. - PubMed
-
- Adams JG, Walls RM. Supporting the health care workforce during the COVID‐19 global epidemic. JAMA 2020; 323: 1439–40. - PubMed
-
- Tsai C. Personal risk and societal obligation amidst COVID‐19. JAMA 2020; 323: 1555–6. - PubMed
-
- Galea S, Merchant RM, Lurie N. The mental health consequences of COVID‐19 and physical distancing. JAMA Intern. Med. 2020; 180: 817. - PubMed