Multicenter Study for the Effect of COVID-19 Lockdown on Patients With Sacral Neuromodulation Implants
Affiliations
Affiliations
- Faculty of Medicine, King Abdulaziz University, Jeddah, Saudi Arabia. Electronic address: drmaibanakher@hotmail.com.
- Department of Urology, King Fahad Specialist Hospital, Dammam, Eastern Province, Saudi Arabia.
- Department of Surgery, Urology Unit, Al-Amiri Hospital, Kuwait City, Kuwait.
- Department of Urology, Austin and Western Health, University of Melbourne, Melbourne, Australia.
- Department of Urology, Toronto Western Hospital (UHN), University of Toronto, Toronto, Canada.
Abstract
Introduction: The massive spread of COVID-19 affected many aspects of medical and surgical services. Many patients with sacral neuromodulation (SNM) devices needed integrated follow-up and close communication regarding the programming of the device. In this study, we aimed to explore the effect of COVID-19 lockdown on patients with SNM devices.
Materials and methods: This was a multicenter study designed and conducted in four centers performing SNM (Toronto Western Hospital, Toronto, Canada; King Abdulaziz University Hospital, Jeddah, Saudi Arabia; Al-Amiri Hospital, Kuwait City, Kuwait; and Austin and Western Health, University of Melbourne, Australia). An online questionnaire was created through Google Forms and circulated among patients with SNM devices in all four mentioned centers. The questionnaire was sent to patients during the forced lockdown period in each country.
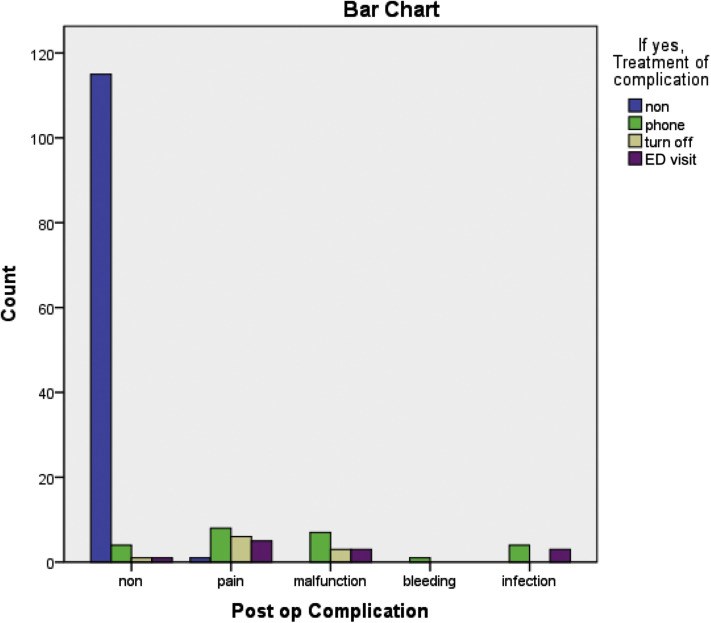
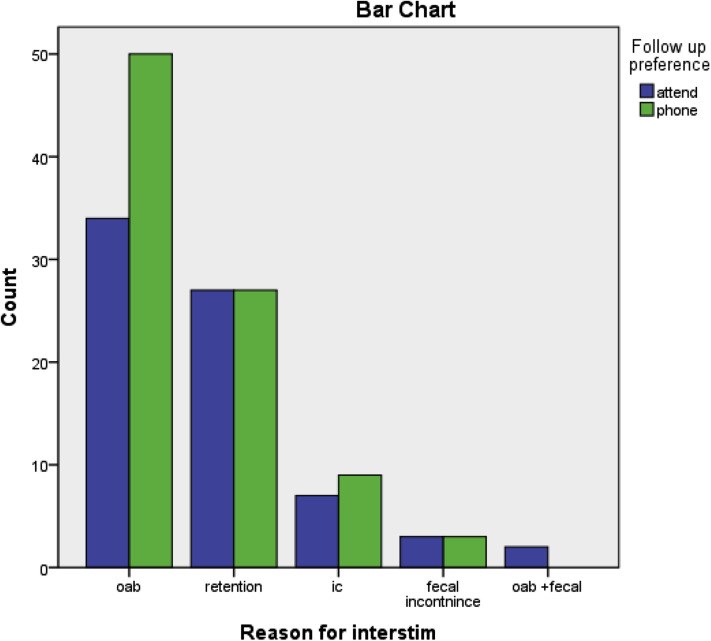
Results: A total of 162 responses were received by September 2020. Data showed that most patients had their device implanted before the lockdown period (92.5%, 150/162). Most patients did not experience any contact difficulties (91.9%, 149/162). When patients were requested for their preference of programming, 89.5% (145/162) preferred remote programming. Correlation analysis did not show any significant relation between patient diagnosis and COVID-19-related difficulties or preferences.
Conclusion: The difficulties with access to care experienced during the pandemic and the patient's expressed willingness to participate in virtual care should provide impetus for manufacturers of SNM devices to move forward with developing remote programming capabilities.
Keywords: COVID-19; LUTS; lockdown; sacral neuromodulation.
Figures
Similar articles
Banakhar MA.Ther Adv Urol. 2021 Jul 20;13:1756287221998135. doi: 10.1177/1756287221998135. eCollection 2021 Jan-Dec.PMID: 34367340 Free PMC article.
Meng L, Hou H, Zhang P, Gu Y, Shi B, Li Y, Wang Q, Zhang Y, Ren L, Chen Q, Yuan Z, Guo F, Li D, Ma Y, Dong S, Liu Z, Shang A, Li B, Xu W, Lv J, Zhang Y.Front Med (Lausanne). 2023 Mar 13;10:977433. doi: 10.3389/fmed.2023.977433. eCollection 2023.PMID: 37035299 Free PMC article.
Outcomes of sacral neuromodulation for chronic pelvic pain: a Finnish national multicenter study.
Zegrea A, Kirss J, Pinta T, Rautio T, Varpe P, Kairaluoma M, Aho M, Böckelman C, Lavonius M.Tech Coloproctol. 2020 Mar;24(3):215-220. doi: 10.1007/s10151-020-02148-2. Epub 2020 Jan 21.PMID: 31965400
Lehur PA, Sørensen M, Dudding TC, Knowles CH, de Wachter S, Engelberg S, Matzel KE; European SNM Expert Group.Neuromodulation. 2020 Dec;23(8):1121-1129. doi: 10.1111/ner.13117. Epub 2020 Mar 9.PMID: 32153080 Free PMC article. Review.
Cohn JA, Kowalik CG, Kaufman MR, Reynolds WS, Milam DF, Dmochowski RR.Expert Rev Med Devices. 2017 Jan;14(1):3-14. doi: 10.1080/17434440.2017.1268913. Epub 2016 Dec 11.PMID: 27915486 Review.
KMEL References
References
-
- Worldometer. COVID-19 Coronavirus Pandemic. Accessed April 2, 2020. https://www.worldometers.info/coronavirus/
-
- World Health Organization . World Health Organization; 2020. Coronavirus Disease (COVID-19) Pandemic.
-
- American Urological Association Information Center Coronavirus disease 2019. https://www.auanet.org/covid-19-info-center/covid-19-info-center Accessed October 29, 2020.
-
- European Association of Urology COVID19 resources for urologists. https://uroweb.org/covid19-resources-for-urologists/ Accessed October 29, 2020.
-
- Fonda D. Coronavirus has ushered in the digital revolution in medicine. How investors can play it. https://www.barrons.com/articles/coronavirus-has-ushered-in-the-teleheal... Accessed May 2, 2020.
-
- Shaw J., Jamieson T., Agarwal P., Griffin B., Wong I., Bhatia R.S. Virtual care policy recommendations for patient-centred primary care: findings of a consensus policy dialogue using a nominal group technique. J Telemed Telecare. 2018;24:608–615. - PubMed
-
- Canadian Medical Association . Canadian Medical Association; 2020. Virtual Care Recommendations for Scaling Up Virtual Medical Services.