Determinants, predictors and negative impacts of burnout among health care workers during COVID-19 pandemic
Affiliations
Affiliations
- The Nephrology Department, Hamed Al-Essa Organ Transplant Center, Ibn Sina Hospital, Sabah Area, Kuwait.
- Chest Department, Faculty of Medicine, Zagazig University, Zagazig, Egypt.
- Department of Dialysis and Transplantation, Urology Nephrology Center, Mansoura University, Mansoura, Egypt.
- Lecturer of Industrial Medicine and Occupational Health, Community, Environmental and Occupational Medicine Department, Faculty of Medicine, Zagazig University, Zagazig, Egypt.
- Clinical Pathology Specialist, National Blood Transfusion Services, Egypt.
- Health Care Management Consultant, Technical Office, MOH, Kuwait.
- Department of Botany and Microbiology, College of Science, King Saud University, P.O. 2455, Riyadh 11451, Saudi Arabia.
- Psychiatry Department, Faculty of Medicine, Zagazig University, Egypt.
- Department of Environmental Sciences, COMSATS University Islamabad, Abbottabad Campus, 22060, Pakistan.
- University of Gastronomic Sciences, Piazza Vittorio Emanuele II, 9, 12042 Pollenzo, Italy.
- Community Medicine Department, Public Health and Preventive Medicine, Faculty of Medicine October 6 University, Giza, Egypt.
Abstract
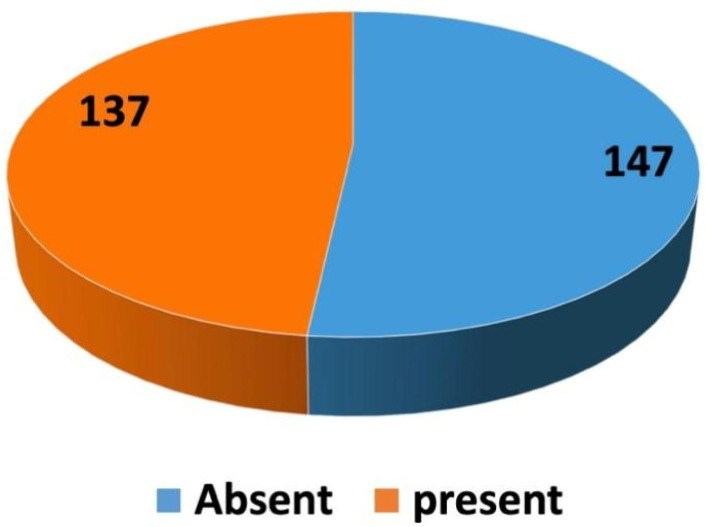
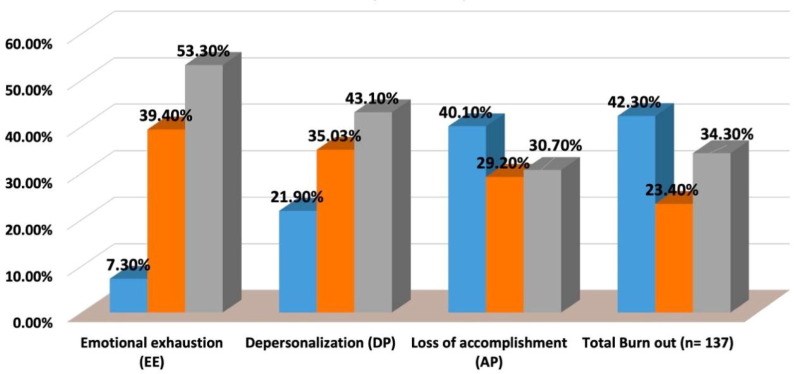
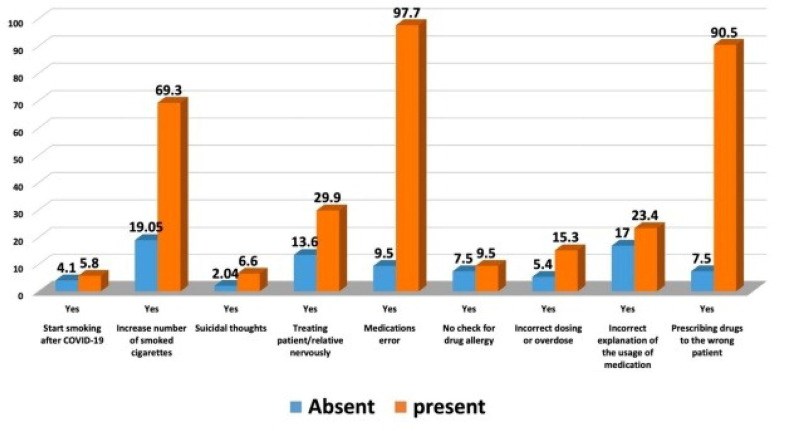
The first defense line of the battle, healthcare workers (HCWs), faces a significant challenge in managing the current COVID-19 pandemic. An online electronic survey was sent to HCWs via email and social media networks. Socio-demographic data and work environment-related variables were assessed. Consequences of burnout (BO) were reported, e.g., elicited medical errors. Maslach burnout inventory was used to diagnose BO. Two hundred and eighty-four participants were included with a mean age of 39.83 ± 7.34 years, 70.8% worked in the COVID-19 frontline, 91.9% were followed daily updates about COVID-19, 63.7% were not satisfied with the coordination between triage and isolation, 64.4% got COVID-19 infection, 91.9% had a colleague or family member developed COVID-19 infection, and 21.5% experienced a colleague /a family member died due to COVID-19. Multivariate analysis by linear regression revealed that; working as a frontline HCW (OR 1.28, CI = 0.14-2.55) and sleep deprivation (OR 3.93, CI = 1.88-8.22) were the predictors of burnout.
Keywords: Burnout; CI, Confidence interval; COVID-19; Maslach Inventory; Medical errors.
Figures
Similar articles
Zhang X, Wang J, Hao Y, Wu K, Jiao M, Liang L, Gao L, Ning N, Kang Z, Shan L, He W, Wang Y, Wu Q, Yin W.Front Psychol. 2021 Aug 16;12:680614. doi: 10.3389/fpsyg.2021.680614. eCollection 2021.PMID: 34484037 Free PMC article.
Youssef D, Abboud E, Abou-Abbas L, Hassan H, Youssef J.J Pharm Policy Pract. 2022 Dec 16;15(1):102. doi: 10.1186/s40545-022-00503-2.PMID: 36527056 Free PMC article.
Stewart NH, Koza A, Dhaon S, Shoushtari C, Martinez M, Arora VM.J Med Internet Res. 2021 May 19;23(5):e27331. doi: 10.2196/27331.PMID: 33875414 Free PMC article.
Stodolska A, Wójcik G, Barańska I, Kijowska V, Szczerbińska K.Int J Occup Med Environ Health. 2023 Mar 2;36(1):21-58. doi: 10.13075/ijomeh.1896.02007. Epub 2023 Feb 2.PMID: 36727492 Review.
Alanazi TNM, McKenna L, Buck M, Alharbi RJ.Australas Emerg Care. 2022 Sep;25(3):197-212. doi: 10.1016/j.auec.2021.10.002. Epub 2021 Nov 12.PMID: 34802977 Free PMC article. Review.
Cited by
Luo M, Xia G, Gan T, Zhao Z, Wu J, Hu T, Wang L, Zhang Y.Front Public Health. 2023 Jul 27;11:1209646. doi: 10.3389/fpubh.2023.1209646. eCollection 2023.PMID: 37575121 Free PMC article.
Robert Selvam D, Xavier S, Kasinathan P, Ahmad Wadaan M, Farooq Khan M, Santha Kumar David M.J King Saud Univ Sci. 2023 May;35(4):102653. doi: 10.1016/j.jksus.2023.102653. Epub 2023 Mar 22.PMID: 36987441 Free PMC article.
KMEL References
References
-
- Abbas A., Ali A., Bahgat S.M., Shouman W. Prevalence, associated factors, and consequences of Burnout among ICU healthcare workers: An Egyptian experience. Egypt. J. Chest Dis. Tuberc. 2019;68(4):514–525.
-
- Chirico F., Nucera G., Magnavita N. Protecting the mental health of healthcare workers during the COVID-19 emergency. B. J. Psych. Int. 2020:1–6.
-
- Duarte I., Teixeira A., Castro L., Marina S., Ribeiro C., Jácome C., Martins V., Ribeiro-Vaz I., Pinheiro H.C., Silva A.R., Ricou M., Sousa B., Alves C., Oliveira A., Silva P., Nunes R., Serrão C. Burnout among Portuguese healthcare workers during the COVID-19 pandemic. BMC Public Health. 2020;20(1):1885. doi: 10.1186/s12889-020-09980-z. - DOI - PMC - PubMed
-
- Gheith O., Maher A., Abbas A., Emam M., Halim M.A., Eldein S.M., et al. Coronavirus 2019 pandemic and renal diseases: a review of the literature. J. Egypt. Soc. Nephrol. Transplant. 2020;20(4):191–203.
-
- Lasalvia A., Amaddeo F., Porru S., Carta A., Tardivo S., Bovo C., Ruggeri M., Bonetto C. Levels of burn-out among healthcare workers during the COVID-19 pandemic and their associated factors: a cross-sectional study in a tertiary hospital of a highly burdened area of north-east Italy. BMJ Open. 2021;11(1):e045127. - PMC - PubMed
-
- Maslach C., Jackson S.E., Leiter M.P. 3rd ed. Consulting Psychologist Press; Palo Alto.; CA: 1996. Maslach Burnout Inventory manual.
-
- Perlis R.H. Exercising Heart and Head in Managing Coronavirus Disease 2019 in Wuhan. JAMA Netw. Open. 2020;3(3):e204006. - PubMed
-
- Sabbah I., Sabbah H., Sabbah S., Akoum H., Droubi N. Burnout among Lebanese nurses: psychometric properties of the Maslach burnout inventory-human services survey (MBI-HSS) Health. 2012;4:644–652.
-
- Wu Y., Wang J., Luo C., Hu S., Lin X., Anderson A.E., Bruera E., Yang X., Wei S., Qian Y. A Comparison of Burnout Frequency Among Oncology Physicians and Nurses Working on the Frontline and Usual Wards During the COVID-19 Epidemic in Wuhan, China. J. Pain Symptom Manag. 2020;60(1):e60–e65. doi: 10.1016/j.jpainsymman.2020.04.008. - DOI - PMC - PubMed