Impact of Antioxidant Therapy on Natural Pregnancy Outcomes and Semen Parameters in Infertile Men: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
Ashok Agarwal 1, Rossella Cannarella 2 3, Ramadan Saleh 4 5, Ahmed M Harraz 6 7 8, Hussein Kandil 9, Gianmaria Salvio 10, Florence Boitrelle 11 12, Shinnosuke Kuroda 3, Ala'a Farkouh 13, Amarnath Rambhatla 14, Armand Zini 15, Giovanni Colpi 16, Murat Gül 17, Parviz Kavoussi 18, Taha Abo-Almagd Abdel-Meguid Hamoda 19 20, Edmund Ko 21, Gokhan Calik 22, Tuncay Toprak 23, Germar-Michael Pinggera 24, Hyun Jun Park 25 26, Ramy Abou Ghayda 27, Suks Minhas 28, Gian Maria Busetto 29, Mustafa Emre Bakırcıoğlu 30, Ates Kadioglu 31, Eric Chung 32, Giorgio Ivan Russo 33, Aldo E Calogero 2, Rafael F Ambar 34 35, Channa N Jayasena 36 37, Rupin Shah 38
Affiliations
Affiliations
- 1American Center for Reproductive Medicine, Global Andrology Forum, Moreland Hills, OH, USA. agarwaa32099@outlook.com.
- 2Department of Clinical and Experimental Medicine, University of Catania, Catania, Italy.
- 3Glickman Urological & Kidney Institute, Cleveland Clinic Foundation, Cleveland, OH, USA.
- 4Department of Dermatology, Venereology and Andrology, Faculty of Medicine, Sohag University, Sohag, Egypt.
- 5Ajyal IVF Center, Ajyal Hospital, Sohag, Egypt.
- 6Department of Urology, Mansoura University Urology and Nephrology Center, Mansoura, Egypt.
- 7Department of Surgery, Urology Unit, Farwaniya Hospital, Farwaniya, Kuwait.
- 8Department of Urology, Sabah Al Ahmad Urology Center, Kuwait City, Kuwait.
- 9Fakih IVF Fertility Center, Abu Dhabi, UAE.
- 10Department of Endocrinology, Polytechnic University of Marche, Ancona, Italy.
- 11Reproductive Biology, Fertility Preservation, Andrology, CECOS, Poissy Hospital, Poissy, France.
- 12Department of Biology, Reproduction, Epigenetics, Environment and Development, Pari. Saclay University, UVSQ, INRAE, BREED, Jouy-en-Josas, France.
- 13American Center for Reproductive Medicine, Global Andrology Forum, Moreland Hills, OH, USA.
- 14Department of Urology, Vattikuti Urology Institute, Henry Ford Health System, Detroit, MI, USA.
- 15Division of Urology, Department of Surgery, McGill University, Montreal, QC, Canada.
- 16Next Fertility Procrea, Lugano, Switzerland.
- 17Department of Urology, Selcuk University School of Medicine, Konya, Turkey.
- 18Austin Fertility & Reproductive Medicine/Westlake IVF, Austin, TX, USA.
- 19Department of Urology, King Abdulaziz University, Jeddah, Saudi Arabia.
- 20Department of Urology, Faculty of Medicine, Minia University, Minia, Egypt.
- 21Department of Urology, Loma Linda University Health, Loma Linda, CA, USA.
- 22Department of Urology, Faculty of Medicine, Istanbul Medipol University, Istanbul, Turkey.
- 23Department of Urology, Fatih Sultan Mehmet Training and Research Hospital, University of Health Sciences, Istanbul, Turkey.
- 24Department of Urology, Medical University Innsbruck, Innsbruck, Austria.
- 25Department of Urology, Pusan National University School of Medicine, Busan, Korea.
- 26Medical Research Institute of Pusan National University Hospital, Busan, Korea.
- 27Urology Institute, University Hospitals, Case Western Reserve University, Cleveland, OH, USA.
- 28Division of Surgery, Department of Surgery and Cancer, Imperial College, London, UK.
- 29Department of Urology and Organ Transplantation, University of Foggia, Ospedali Riuniti of Foggia, Foggia, Italy.
- 30SENSART Clinic, Istanbul, Turkey.
- 31Section of Andrology, Department of Urology, Istanbul Faculty of Medicine, Istanbul University, Istanbul, Turkey.
- 32Department of Urology, Princess Alexandra Hospital, University of Queensland, Brisbane, Australia.
- 33Urology Section, University of Catania, Catania, Italy.
- 34Department of Urology, Centro Universitario em Saude do ABC, Santo André, Brazil.
- 35Andrology Group at Ideia Fertil Institute of Human Reproduction, Santo André, Brazil.
- 36Department of Reproductive Endocrinology and Andrology, Imperial College London, London, UK.
- 37Department of Andrology, Hammersmith & St. Mary's Hospitals, London, UK.
- 38Division of Andrology, Department of Urology, Lilavati Hospital and Research Centre, Mumbai, India.
Abstract
Purpose: Seminal oxidative stress (OS) is a recognized factor potentially associated with male infertility, but the efficacy of antioxidant (AOX) therapy is controversial and there is no consensus on its utility. Primary outcomes of this study were to investigate the effect of AOX on spontaneous clinical pregnancy, live birth and miscarriage rates in male infertile patients. Secondary outcomes were conventional semen parameters, sperm DNA fragmentation (SDF) and seminal OS.
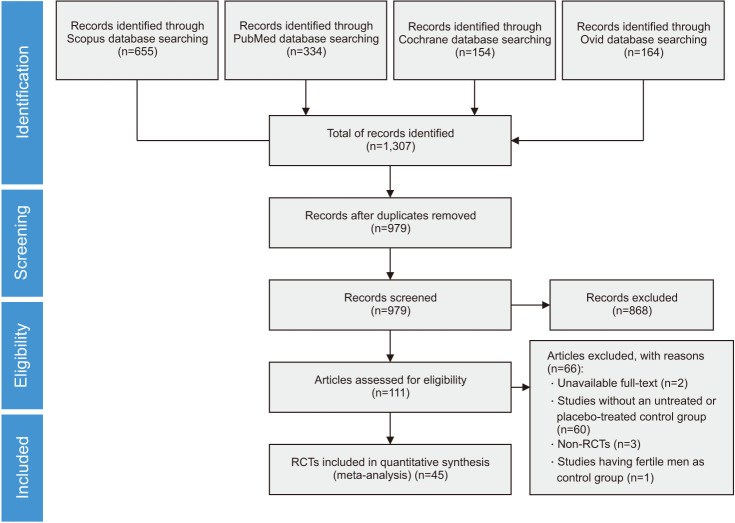
Materials and methods: Literature search was performed using Scopus, PubMed, Ovid, Embase, and Cochrane databases. Only randomized controlled trials (RCTs) were included and the meta-analysis was conducted according to PRISMA guidelines.
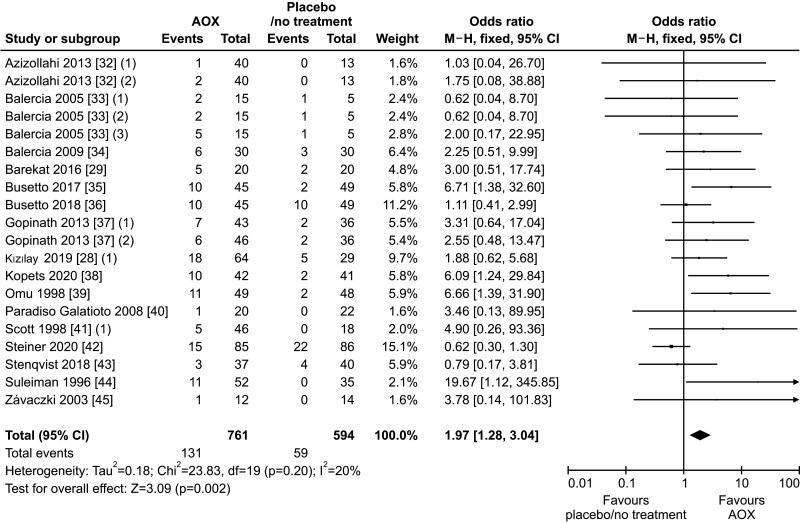
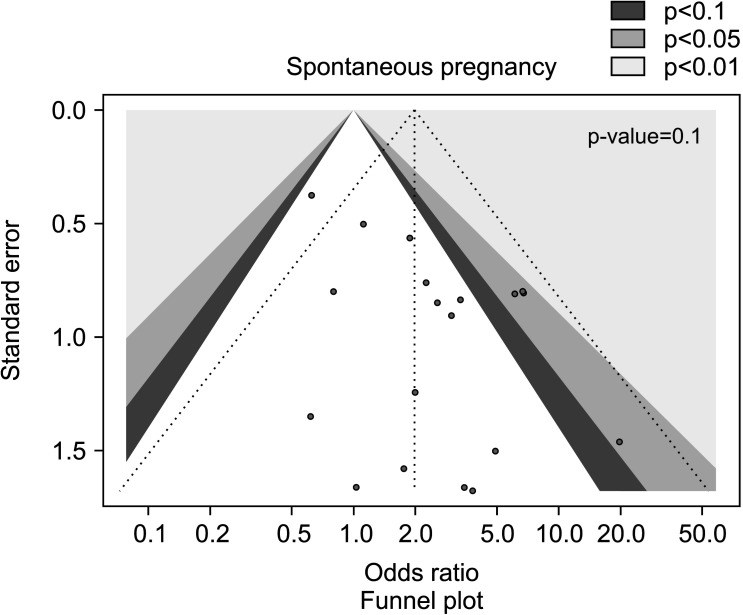
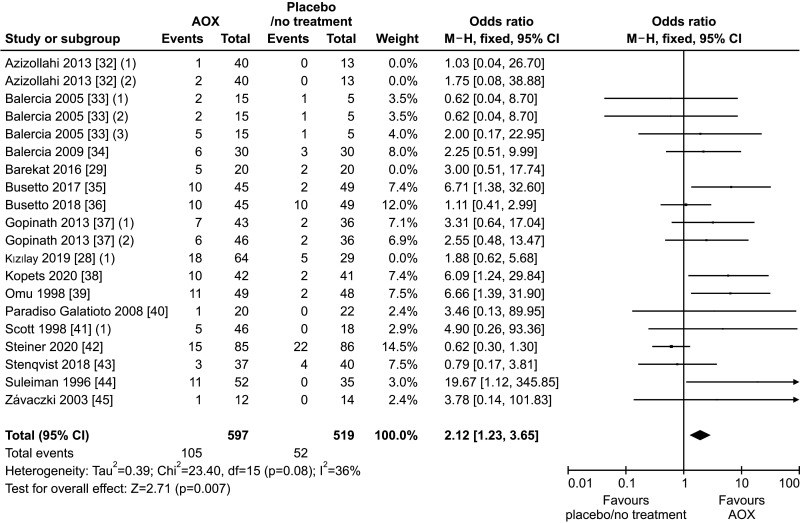
Results: We assessed for eligibility 1,307 abstracts, and 45 RCTs were finally included, for a total of 4,332 infertile patients. We found a significantly higher pregnancy rate in patients treated with AOX compared to placebo-treated or untreated controls, without significant inter-study heterogeneity. No effects on live-birth or miscarriage rates were observed in four studies. A significantly higher sperm concentration, sperm progressive motility, sperm total motility, and normal sperm morphology was found in patients compared to controls. We found no effect on SDF in analysis of three eligible studies. Seminal levels of total antioxidant capacity were significantly higher, while seminal malondialdehyde acid was significantly lower in patients than controls. These results did not change after exclusion of studies performed following varicocele repair.
Conclusions: The present analysis upgrades the level of evidence favoring a recommendation for using AOX in male infertility to improve the spontaneous pregnancy rate and the conventional sperm parameters. The failure to demonstrate an increase in live-birth rate, despite an increase in pregnancy rates, is due to the very few RCTs specifically assessing the impact of AOX on live-birth rate. Therefore, further RCTs assessing the impact of AOX on live-birth rate and miscarriage rate, and SDF will be helpful.
Keywords: Antioxidants; Male infertility; Meta-analysis; Pregnancy; Semen parameters; Sperm DNA fragmentation.
Conflict of interest statement
The authors have nothing to disclose.
Figures
Similar articles
Antioxidants for male subfertility.
Showell MG, Mackenzie-Proctor R, Brown J, Yazdani A, Stankiewicz MT, Hart RJ.Cochrane Database Syst Rev. 2014;(12):CD007411. doi: 10.1002/14651858.CD007411.pub3. Epub 2014 Dec 15.PMID: 25504418 Updated. Review.
Agarwal A, Cannarella R, Saleh R, Boitrelle F, Gül M, Toprak T, Salvio G, Arafa M, Russo GI, Harraz AM, Singh R, Garrido N, Hamoda TAA, Rambhatla A, Kavoussi P, Kuroda S, Çalik G, Saini P, Ceyhan E, Dimitriadis F, Henkel R, Crafa A, Palani A, Duran MB, Maziotis E, Saïs É, Bendayan M, Darbandi M, Le TV, Gunes S, Tsioulou P, Sengupta P, Hazir B, Çeker G, Darbandi S, Durairajanayagam D, Aghamajidi A, Alkhalidi N, Sogutdelen E, Leisegang K, Alarbid A, Ho CCK, Malhotra V, Finocchi F, Crisóstomo L, Kosgi R, ElBardisi H, Zini A, Birowo P, Colpi G, Park HJ, Serefoglu EC, Nguyen Q, Ko E, de la Rosette J, Pinggera GM, Nguyen HVP, Kandil H, Shah R.World J Mens Health. 2023 Apr;41(2):289-310. doi: 10.5534/wjmh.220142. Epub 2022 Oct 28.PMID: 36326166 Free PMC article.
Antioxidants for male subfertility.
Smits RM, Mackenzie-Proctor R, Yazdani A, Stankiewicz MT, Jordan V, Showell MG.Cochrane Database Syst Rev. 2019 Mar 14;3(3):CD007411. doi: 10.1002/14651858.CD007411.pub4.PMID: 30866036 Free PMC article. Updated.
Yan X, Dong L, Liu Y, Yang F, Tan K, Li J, Chang D, Yu X.Medicine (Baltimore). 2019 Oct;98(41):e17494. doi: 10.1097/MD.0000000000017494.PMID: 31593115 Free PMC article.
Ata B, Abou-Setta AM, Seyhan A, Buckett W.Cochrane Database Syst Rev. 2018 Feb 28;2(2):CD011809. doi: 10.1002/14651858.CD011809.pub2.PMID: 29489026 Free PMC article. Review.
Cited by
Role of oxidative stress in male infertility.
Takalani NB, Monaneng EM, Mohlala K, Monsees TK, Henkel R, Opuwari CS.Reprod Fertil. 2023 Jul 7;4(3):e230024. doi: 10.1530/RAF-23-0024.PMID: 37276172 Free PMC article. Review.
Zafar MI, Mills KE, Baird CD, Jiang H, Li H.Drugs. 2023 Apr;83(6):531-546. doi: 10.1007/s40265-023-01853-0. Epub 2023 Mar 21.PMID: 36943634
Zhang QF, Wang S, Zhang H, Liu QL, Wei Y, Deng W, Wang C, Yang B.Trials. 2022 Dec 12;23(1):1002. doi: 10.1186/s13063-022-06951-0.PMID: 36510262 Free PMC article.
Coenzyme Q10 and Melatonin for the Treatment of Male Infertility: A Narrative Review.
Lucignani G, Jannello LMI, Fulgheri I, Silvani C, Turetti M, Gadda F, Viganò P, Somigliana E, Montanari E, Boeri L.Nutrients. 2022 Nov 1;14(21):4585. doi: 10.3390/nu14214585.PMID: 36364847 Free PMC article. Review.
KMEL References
References
-
- Agarwal A, Baskaran S, Parekh N, Cho CL, Henkel R, Vij S, et al. Male infertility. Lancet. 2021;397:319–333. - PubMed
-
- Irvine DS. Epidemiology and aetiology of male infertility. Hum Reprod. 1998;13 Suppl 1:33–44. - PubMed
-
- Salonia A, Bettocchi C, Boeri L, Capogrosso P, Carvalho J, Cilesiz NC, et al. EAU Working Group on Male Sexual and reproductive health. European Association of Urology guidelines on sexual and reproductive health-2021 update: male sexual dysfunction. Eur Urol. 2021;80:333–357. - PubMed
-
- Sharma RK, Agarwal A. Role of reactive oxygen species in male infertility. Urology. 1996;48:835–850. - PubMed
-
- Bui AD, Sharma R, Henkel R, Agarwal A. Reactive oxygen species impact on sperm DNA and its role in male infertility. Andrologia. 2018;50:e13012. - PubMed
-
- Aitken RJ. Reactive oxygen species as mediators of sperm capacitation and pathological damage. Mol Reprod Dev. 2017;84:1039–1052. - PubMed
-
- Alvarez JG, Storey BT. Differential incorporation of fatty acids into and peroxidative loss of fatty acids from phospholipids of human spermatozoa. Mol Reprod Dev. 1995;42:334–346. - PubMed
-
- Barati E, Nikzad H, Karimian M. Oxidative stress and male infertility: current knowledge of pathophysiology and role of antioxidant therapy in disease management. Cell Mol Life Sci. 2020;77:93–113. - PubMed
-
- Ali M, Martinez M, Parekh N. Are antioxidants a viable treatment option for male infertility? Andrologia. 2021;53:e13644. - PubMed
-
- Zhang X, Cui Y, Dong L, Sun M, Zhang Y. The efficacy of combined l-carnitine and l-acetyl carnitine in men with idiopathic oligoasthenoteratozoospermia: a systematic review and meta-analysis. Andrologia. 2020;52:e13470. - PubMed
-
- Wang J, Wang T, Ding W, Wu J, Wu G, Wang Y, et al. Efficacy of antioxidant therapy on sperm quality measurements after varicocelectomy: a systematic review and meta-analysis. Andrologia. 2019;51:e13396. - PubMed
-
- Bahmyari R, Zare M, Sharma R, Agarwal A, Halvaei I. The efficacy of antioxidants in sperm parameters and production of reactive oxygen species levels during the freeze-thaw process: a systematic review and meta-analysis. Andrologia. 2020;52:e13514. - PubMed
-
- Salonia A, Bettocchi C, Carvalho J, Corona G, Jones TH, Kadioğlu A, et al. Sexual and reproductive health. Vol. 282 Arnhem: European Association of Urology; 2022.
-
- Schlegel PN, Sigman M, Collura B, De Jonge CJ, Eisenberg ML, Lamb DJ, et al. Diagnosis and treatment of infertility in men: AUA/ASRM guideline part I. J Urol. 2021;205:36–43. - PubMed
-
- Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;350:g7647. - PubMed
-
- Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. - PubMed
-
- Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12. - PubMed
-
- Ardestani Zadeh A, Arab D, Kia NS, Heshmati S, Amirkhalili SN. The role of vitamin E - selenium - folic acid supplementation in improving sperm parameters after varicocelectomy: a randomized clinical trial. Urol J. 2019;16:495–500. - PubMed
-
- Kızılay F, Altay B. Evaluation of the effects of antioxidant treatment on sperm parameters and pregnancy rates in infertile patients after varicocelectomy: a randomized controlled trial. Int J Impot Res. 2019;31:424–431. - PubMed
-
- Ener K, Aldemir M, Işık E, Okulu E, Özcan MF, Uğurlu M, et al. The impact of vitamin E supplementation on semen parameters and pregnancy rates after varicocelectomy: a randomised controlled study. Andrologia. 2016;48:829–834. - PubMed
-
- Balercia G, Regoli F, Armeni T, Koverech A, Mantero F, Boscaro M. Placebo-controlled double-blind randomized trial on the use of L-carnitine, L-acetylcarnitine, or combined L-carnitine and L-acetylcarnitine in men with idiopathic asthenozoospermia. Fertil Steril. 2005;84:662–671. - PubMed
-
- Balercia G, Buldreghini E, Vignini A, Tiano L, Paggi F, Amoroso S, et al. Coenzyme Q10 treatment in infertile men with idiopathic asthenozoospermia: a placebo-controlled, double-blind randomized trial. Fertil Steril. 2009;91:1785–1792. - PubMed
-
- Busetto GM, Virmani A, Antonini G, Ragonesi G, Del Giudice F, Agarwal A, et al. Effect of antioxidant supplementation on sperm parameters in oligo-astheno-teratozoospermia, with and without varicocele: a double blind place controlled (DBPC) study. Eur Urol Suppl. 2017;16:e782 - PubMed
-
- Busetto GM, Agarwal A, Virmani A, Antonini G, Ragonesi G, Del Giudice F, et al. Effect of metabolic and antioxidant supplementation on sperm parameters in oligo-astheno-teratozoospermia, with and without varicocele: a double-blind placebo-controlled study. Andrologia. 2018;50:e12927 - PubMed
-
- Gopinath PM, Kalra B, Saxena A, Malik S, Kochhar K, Kalra S, et al. Fixed dose combination therapy of antioxidants in treatment of idiopathic oligoasthenozoospermia: results of a randomized, double-blind, placebo-controlled clinical trial. IJIFM. 2013;4:6–13.
-
- Kopets R, Kuibida I, Chernyavska I, Cherepanyn V, Mazo R, Fedevych V, et al. Dietary supplementation with a novel l-carnitine multi-micronutrient in idiopathic male subfertility involving oligo-, astheno-, teratozoospermia: a randomized clinical study. Andrology. 2020;8:1184–1193. - PubMed
-
- Omu AE, Dashti H, Al-Othman S. Treatment of asthenozoospermia with zinc sulphate: andrological, immunological and obstetric outcome. Eur J Obstet Gynecol Reprod Biol. 1998;79:179–184. - PubMed
-
- Paradiso Galatioto G, Gravina GL, Angelozzi G, Sacchetti A, Innominato PF, Pace G, et al. May antioxidant therapy improve sperm parameters of men with persistent oligospermia after retrograde embolization for varicocele? World J Urol. 2008;26:97–102. - PubMed
-
- Scott R, MacPherson A, Yates RW, Hussain B, Dixon J. The effect of oral selenium supplementation on human sperm motility. Br J Urol. 1998;82:76–80. - PubMed
-
- Stenqvist A, Oleszczuk K, Leijonhufvud I, Giwercman A. Impact of antioxidant treatment on DNA fragmentation index: a double-blind placebo-controlled randomized trial. Andrology. 2018;6:811–816. - PubMed
-
- Suleiman SA, Ali ME, Zaki ZM, el-Malik EM, Nasr MA. Lipid peroxidation and human sperm motility: protective role of vitamin E. J Androl. 1996;17:530–537. - PubMed
-
- Závaczki Z, Szöllõsi J, Kiss SA, Koloszár S, Fejes I, Kovács L, et al. Magnesium-orotate supplementation for idiopathic infertile male patients: a randomized, placebo-controlled clinical pilot study. Magnes Res. 2003;16:131–136. - PubMed
-
- Boonyarangkul A, Vinayanuvattikhun N, Chiamchanya C, Visutakul P. Comparative study of the effects of tamoxifen citrate and folate on semen quality of the infertile male with semen abnormality. J Med Assoc Thai. 2015;98:1057–1063. - PubMed
-
- Ciftci H, Verit A, Savas M, Yeni E, Erel O. Effects of N-acetylcysteine on semen parameters and oxidative/antioxidant status. Urology. 2009;74:73–76. - PubMed
-
- Conquer JA, Martin JB, Tummon I, Watson L, Tekpetey F. Effect of DHA supplementation on DHA status and sperm motility in asthenozoospermic males. Lipids. 2000;35:149–154. - PubMed
-
- da Silva TM, Maia MCS, Arruda JT, Approbato FC, Mendonça CR, Approbato MS. Folic acid does not improve semen parametrs in subfertile men: a double-blin, randomized, placebo-controlled study. JBRA Assist Reprod. 2013;17:152–157.
-
- Dimitriadis F, Tsambalas S, Tsounapi P, Kawamura H, Vlachopoulou E, Haliasos N, et al. Effects of phosphodiesterase-5 inhibitors on Leydig cell secretory function in oligoasthenospermic infertile men: a randomized trial. BJU Int. 2010;106:1181–1185. - PubMed
-
- Eslamian G, Amirjannati N, Noori N, Sadeghi MR, Hekmatdoost A. Effects of coadministration of DHA and vitamin E on spermatogram, seminal oxidative stress, and sperm phospholipids in asthenozoospermic men: a randomized controlled trial. Am J Clin Nutr. 2020;112:707–719. - PubMed
-
- Greco E, Iacobelli M, Rienzi L, Ubaldi F, Ferrero S, Tesarik J. Reduction of the incidence of sperm DNA fragmentation by oral antioxidant treatment. J Androl. 2005;26:349–353. - PubMed
-
- Haghighian HK, Haidari F, Mohammadi-Asl J, Dadfar M. Randomized, triple-blind, placebo-controlled clinical trial examining the effects of alpha-lipoic acid supplement on the spermatogram and seminal oxidative stress in infertile men. Fertil Steril. 2015;104:318–324. - PubMed
-
- Lenzi A, Lombardo F, Sgrò P, Salacone P, Caponecchia L, Dondero F, et al. Use of carnitine therapy in selected cases of male factor infertility: a double-blind crossover trial. Fertil Steril. 2003;79:292–300. - PubMed
-
- Lu XL, Liu JJ, Li JT, Yang QA, Zhang JM. Melatonin therapy adds extra benefit to varicecelectomy in terms of sperm parameters, hormonal profile and total antioxidant capacity: a placebo-controlled, double-blind trial. Andrologia. 2018;50:e13033. - PubMed
-
- Martinez-Soto JC, Domingo JC, Cordobilla B, Palbero L, Pellicer A, Landeras J. Effect of dietary DHA supplementation on sperm DNA integrity. Fertil Steril. 2010;94:S235–S236.
-
- Morgante G, Scolaro V, Tosti C, Di Sabatino A, Piomboni P, De Leo V. [Treatment with carnitine, acetyl carnitine, L-arginine and ginseng improves sperm motility and sexual health in men with asthenopermia] Minerva Urol Nefrol. 2010;62:213–218. - PubMed
-
- Nadjarzadeh A, Sadeghi MR, Amirjannati N, Vafa MR, Motevalian SA, Gohari MR, et al. Coenzyme Q10 improves seminal oxidative defense but does not affect on semen parameters in idiopathic oligoasthenoteratozoospermia: a randomized double-blind, placebo controlled trial. J Endocrinol Invest. 2011;34:e224–e228. - PubMed
-
- Nouri M, Amani R, Nasr-Esfahani M, Tarrahi MJ. The effects of lycopene supplement on the spermatogram and seminal oxidative stress in infertile men: a randomized, double-blind, placebo-controlled clinical trial. Phytother Res. 2019;33:3203–3211. - PubMed
-
- Omu AE, Al-Azemi MK, Kehinde EO, Anim JT, Oriowo MA, Mathew TC. Indications of the mechanisms involved in improved sperm parameters by zinc therapy. Med Princ Pract. 2008;17:108–116. - PubMed
-
- Peivandi S, Karimpour A, Moslemizadeh N. Effects of L-carnitine on infertile men’s spermogram; a randomized clinical trial. J Reprod Infertil. 2010;10:245–251.
-
- Rolf C, Cooper TG, Yeung CH, Nieschlag E. Antioxidant treatment of patients with asthenozoospermia or moderate oligoasthenozoospermia with high-dose vitamin C and vitamin E: a randomized, placebo-controlled, double-blind study. Hum Reprod. 1999;14:1028–1033. - PubMed
-
- Safarinejad MR, Safarinejad S, Shafiei N, Safarinejad S. Effects of the reduced form of coenzyme Q10 (ubiquinol) on semen parameters in men with idiopathic infertility: a double-blind, placebo controlled, randomized study. J Urol. 2012;188:526–531. - PubMed
-
- Safarinejad MR. Effect of omega-3 polyunsaturated fatty acid supplementation on semen profile and enzymatic anti-oxidant capacity of seminal plasma in infertile men with idiopathic oligoasthenoteratospermia: a double-blind, placebo-controlled, randomised study. Andrologia. 2011;43:38–47. - PubMed
-
- Safarinejad MR, Safarinejad S. Efficacy of selenium and/or N-acetyl-cysteine for improving semen parameters in infertile men: a double-blind, placebo controlled, randomized study. J Urol. 2009;181:741–751. - PubMed
-
- Safarinejad MR. Efficacy of coenzyme Q10 on semen parameters, sperm function and reproductive hormones in infertile men. J Urol. 2009;182:237–248. - PubMed
-
- Stanislavov R, Nikolova V, Rohdewald P. Improvement of seminal parameters with Prelox: a randomized, double-blind, placebo-controlled, cross-over trial. Phytother Res. 2009;23:297–302. - PubMed
-
- Blomberg Jensen M, Lawaetz JG, Petersen JH, Juul A, Jørgensen N. Effects of vitamin D supplementation on semen quality, reproductive hormones, and live birth rate: a randomized clinical trial. J Clin Endocrinol Metab. 2018;103:870–881. - PubMed
-
- Dawson EB, Harris WA, Powell LC. Relationship between ascorbic acid and male fertility. World Rev Nutr Diet. 1990;62:1–26. - PubMed
-
- Sigman M, Glass S, Campagnone J, Pryor JL. Carnitine for the treatment of idiopathic asthenospermia: a randomized, double-blind, placebo-controlled trial. Fertil Steril. 2006;85:1409–1414. - PubMed
-
- Ross C, Morriss A, Khairy M, Khalaf Y, Braude P, Coomarasamy A, et al. A systematic review of the effect of oral antioxidants on male infertility. Reprod Biomed Online. 2010;20:711–723. - PubMed
-
- Muratori M, Marchiani S, Tamburrino L, Baldi E. Sperm DNA fragmentation: mechanisms of origin. Adv Exp Med Biol. 2019;1166:75–85. - PubMed
-
- Jannatifar R, Cheraghi E, Nasr-Esfahani MH, Piroozmanesh H. Association of heat shock protein A2 expression and sperm quality after N-acetyl-cysteine supplementation in asthenoterato-zoospermic infertile men. Andrologia. 2021;53:e14024. - PubMed
-
- Pourmand G, Movahedin M, Dehghani S, Mehrsai A, Ahmadi A, Pourhosein M, et al. Does L-carnitine therapy add any extra benefit to standard inguinal varicocelectomy in terms of deoxyribonucleic acid damage or sperm quality factor indices: a randomized study. Urology. 2014;84:821–825. - PubMed
-
- Huang WJ, Lu XL, Li JT, Zhang JM. Effects of folic acid on oligozoospermia with MTHFR polymorphisms in term of seminal parameters, DNA fragmentation, and live birth rate: a double-blind, randomized, placebo-controlled trial. Andrology. 2020;8:110–116. - PubMed
-
- Schisterman EF, Sjaarda LA, Clemons T, Carrell DT, Perkins NJ, Johnstone E, et al. Effect of folic acid and zinc supplementation in men on semen quality and live birth among couples undergoing infertility treatment: a randomized clinical trial. JAMA. 2020;323:35–48. Erratum in: JAMA 2020;323:1194. - PMC - PubMed
-
- Gupta S, Finelli R, Agarwal A, Henkel R. Total antioxidant capacity-Relevance, methods and clinical implications. Andrologia. 2021;53:e13624. - PubMed
-
- Comhaire FH, Christophe AB, Zalata AA, Dhooge WS, Mahmoud AM, Depuydt CE. The effects of combined conventional treatment, oral antioxidants and essential fatty acids on sperm biology in subfertile men. Prostaglandins Leukot Essent Fatty Acids. 2000;63:159–165. - PubMed
-
- Keskes-Ammar L, Feki-Chakroun N, Rebai T, Sahnoun Z, Ghozzi H, Hammami S, et al. Sperm oxidative stress and the effect of an oral vitamin E and selenium supplement on semen quality in infertile men. Arch Androl. 2003;49:83–94. - PubMed
-
- Halliwell B. The antioxidant paradox. Lancet. 2000;355:1179–1180. - PubMed
-
- Zhou Z, Cui Y, Zhang X, Zhang Y. The role of N-acetyl-cysteine (NAC) orally daily on the sperm parameters and serum hormones in idiopathic infertile men: a systematic review and meta-analysis of randomised controlled trials. Andrologia. 2021;53:e13953. - PubMed
-
- Showell MG, Mackenzie-Proctor R, Brown J, Yazdani A, Stankiewicz MT, Hart RJ. Antioxidants for male subfertility. Cochrane Database Syst Rev. 2014;12:CD007411 - PubMed
-
- Su JS, Farber NJ, Vij SC. Pathophysiology and treatment options of varicocele: an overview. Andrologia. 2021;53:e13576. - PubMed
-
- Colpi GM, Francavilla S, Haidl G, Link K, Behre HM, Goulis DG, et al. European Academy of Andrology guideline management of oligo-astheno-teratozoospermia. Andrology. 2018;6:513–524. - PubMed
-
- Ferlin A, Calogero AE, Krausz C, Lombardo F, Paoli D, Rago R, et al. Management of male factor infertility: position statement from the Italian Society of Andrology and Sexual Medicine (SIAMS): endorsing organization: Italian Society of Embryology, Reproduction, and Research (SIERR) J Endocrinol Invest. 2022;45:1085–1113. - PubMed
-
- European Association of Urology. Sexual and reproductive health [Internet] Arnhem: European Association of Urology; c2022. [cited 2022 Apr 12]. Available from: https://uroweb.org/guidelines/sexual-and-reproductive-health.