Impact of Varicocele Repair on Semen Parameters in Infertile Men: A Systematic Review and Meta-Analysis
Ashok Agarwal 1, Rossella Cannarella 2 3, Ramadan Saleh 4, Florence Boitrelle 5 6, Murat Gül 7, Tuncay Toprak 8, Gianmaria Salvio 9, Mohamed Arafa 10 11, Giorgio I Russo 12, Ahmed M Harraz 13 14 15, Rajender Singh 16, Nicolas Garrido 17, Taha Abo-Almagd Abdel-Meguid Hamoda 18 19, Amarnath Rambhatla 20, Parviz Kavoussi 21, Shinnosuke Kuroda 3, Gökhan Çalik 22, Pallavi Saini 16, Erman Ceyhan 23, Fotios Dimitriadis 24, Ralf Henkel 25 26 27, Andrea Crafa 2, Ayad Palani 28, Mesut Berkan Duran 29, Evangelos Maziotis 30 31, Émine Saïs 5 6, Marion Bendayan 5 6, Mahsa Darbandi 32 33, Tan V Le 34 35, Sezgin Gunes 36, Petroula Tsioulou 30, Pallav Sengupta 37, Berk Hazir 38, Gökhan Çeker 39 40, Sara Darbandi 32 33, Damayanthi Durairajanayagam 41, Azin Aghamajidi 42, Noora Alkhalidi 43, Emrullah Sogutdelen 44, Kristian Leisegang 45, Abdullah Alarbid 14, Christopher C K Ho 46, Vineet Malhotra 47, Federica Finocchi 9 48, Luís Crisóstomo 49 50 51, Raghavender Kosgi 52, Haitham ElBardisi 10 11, Armand Zini 53, Ponco Birowo 54, Giovanni Colpi 55, Hyun Jun Park 56 57, Ege Can Serefoglu 58, Quang Nguyen 59 60, Edmund Ko 61, Jean de la Rosette 62, Germar M Pinggera 63, Ho Vinh Phuoc Nguyen 34 35, Hussein Kandil 64, Rupin Shah 65
Affiliations
Affiliations
- Global Andrology Forum, American Center for Reproductive Medicine, Moreland Hills, OH, USA. agarwaa32099@outlook.com.
- 2Department of Clinical and Experimental Medicine, University of Catania, Catania, Italy.
- 3Glickman Urological & Kidney Institute, Cleveland Clinic Foundation, Cleveland, OH, USA.
- 4Department of Dermatology, Venereology and Andrology, Faculty of Medicine, Sohag University, Sohag, Egypt.
- 5Department of Reproductive Biology, Fertility Preservation, Andrology, CECOS, Poissy Hospital, Poissy, France.
- 6Department of Biology, Reproduction, Epigenetics, Environment and Development, Paris Saclay University, UVSQ, INRAE, BREED, Jouy-en-Josas, France.
- 7Department of Urology, Selcuk University School of Medicine, Konya, Türkiye.
- 8Department of Urology, Fatih Sultan Mehmet Training and Research Hospital, University of Health Sciences, Istanbul, Türkiye.
- 9Department of Endocrinology, Polytechnic University of Marche, Ancona, Italy.
- 10Department of Urology, Hamad Medical Corporation, Doha, Qatar.
- 11Department of Urology, Weill Cornell Medical-Qatar, Doha, Qatar.
- 12Urology Section, University of Catania, Catania, Italy.
- 13Mansoura University Urology and Nephrology Center, Mansoura, Egypt.
- 14Department of Surgery, Urology Unit, Farwaniya Hospital, Farwaniya, Kuwait.
- 15Department of Urology, Sabah Al Ahmad Urology Center, Kuwait City, Kuwait.
- 16Division of Endocrinology, Central Drug Research Institute, Lucknow, India.
- 17IVI Foundation, Instituto de Investigación Sanitaria La Fe (IIS La Fe), Valencia, Spain.
- 18Department of Urology, King Abdulaziz University, Jeddah, Saudi Arabia.
- 19Department of Urology, Faculty of Medicine, Minia University, Minia, Egypt.
- 20Department of Urology, Vattikuti Urology Institute, Henry Ford Health System, Detroit, MI, USA.
- 21Austin Fertility & Reproductive Medicine/Westlake IVF, Austin, TX, USA.
- 22Department of Urology, Faculty of Medicine, Istanbul Medipol University, Istanbul, Türkiye.
- 23Department of Urology, Baskent University Faculty of Medicine, Ankara, Türkiye.
- 24Department of Urology, Medical School, Aristotle University of Thessaloniki, Thessaloniki, Greece.
- 25Department of Metabolism, Digestion and Reproduction, Imperial College London, London, UK.
- 26Department of Medical Bioscience, University of the Western Cape, Bellville, South Africa.
- 27LogixX Pharma, Theale, Berkshire, UK.
- 28Research Centre, University of Garmian, Kalar, Iraq.
- 29Department of Urology, School of Medicine, Pamukkale University, Denizli, Türkiye.
- 30Laboratory of Physiology, Medical School, National and Kapodistrian University of Athens, Athens, Greece.
- 31Assisted Reproduction Unit, Second Department of Obstetrics and Gynecology, Aretaieion Hospital, Medical School, National and Kapodistrian University of Athens, Athens, Greece.
- 32Fetal Health Research Center, Hope Generation Foundation, Tehran, Iran.
- 33Gene Therapy and Regenerative Medicine Research Center, Hope Generation Foundation, Tehran, Iran.
- 34Department of Andrology, Binh Dan Hospital, Ho Chi Minh City, Vietnam.
- 35Department of Urology and Andrology, Pham Ngoc Thach University of Medicine, Ho Chi Minh City, Vietnam.
- 36Department of Medical Biology, Faculty of Medicine, Ondokuz Mayis University, Samsun, Türkiye.
- 37Department of Biomedical Sciences, College of Medicine, Gulf Medical University, Ajman, UAE.
- 38Reproductive Medicine, Department of Translational Medicine, Lund University, Malmö, Sweden.
- 39Department of Urology, Başakşehir Çam and Sakura City Hospital, Istanbul, Türkiye.
- 40Department of Embryology and Histology, Zonguldak Bülent Ecevit University Institute of Health Sciences, Zonguldak, Türkiye.
- 41Department of Physiology, Faculty of Medicine, Universiti Teknologi MARA, Sungai Buloh Campus, Selangor, Malaysia.
- 42Department of Immunology, School of Medicine, Iran University of Medical Sciences, Tehran, Iran.
- 43Department of Internal Medicine, Trinity Health/Mercy Health, Muskegon, MI, USA.
- 44Department of Urology, Bolu Abant Izzet Baysal University, Bolu, Türkiye.
- 45School of Natural Medicine, Faculty of Community and Health Sciences, University of the Western Cape, Bellville, South Africa.
- 46Department of Surgery, School of Medicine, Faculty of Health and Medical Sciences, Taylor's University, Subang Jaya, Malaysia.
- 47Department of Urology and Andrology, VNA Hospital, New Delhi, India.
- 48Unit of Andrology and Reproductive Medicine, Department of Medicine, University of Padua, Padua, Italy.
- 49Unidade Multidisciplinar de Investigação Biomédica (UMIB), Instituto de Ciências Biomédicas Abel Salazar (ICBAS), Universidade do Porto, Porto, Portugal.
- 50Laboratory for Integrative and Translational Research in Population Health (ITR), Universidade do Porto, Porto, Portugal.
- 51Institute of Biomedicine, University of Turku, Turku, Finland.
- 52Department of Urology and Andrology, AIG Hospitals, Gachibowli, Hyderabad, India.
- 53Department of Surgery, McGill University, Montreal, QC, Canada.
- 54Department of Urology, Cipto Mangunkusumo General Hospital, Faculty of Medicine, Universitas Indonesia, Jakarta, Indonesia.
- 55Andrology and IVF Center, Next Fertility Procrea, Lugano, Switzerland.
- 56Department of Urology, Pusan National University School of Medicine, Busan, Korea.
- 57Medical Research Institute of Pusan National University Hospital, Busan, Korea.
- 58Department of Urology, Biruni University School of Medicine, Istanbul, Türkiye.
- 59Center for Andrology and Sexual Medicine, Viet Duc University Hospital, Hanoi, Vietnam.
- 60Department of Urology, Andrology and Sexual Medicine, University of Medicine and Pharmacy, Vietnam National University, Hanoi, Vietnam.
- 61Department of Urology, Loma Linda University Health, Loma Linda, CA, USA.
- 62Department of Urology, Faculty of Medicine, Istanbul Medipol Mega University Hospital, Istanbul, Türkiye.
- 63Department of Urology, Innsbruck Medical University, Innsbruck, Austria.
- 64Fakih IVF Fertility Center, Abu Dhabi, UAE.
- 65Division of Andrology, Department of Urology, Lilavati Hospital and Research Centre, Mumbai, India.
Abstract
Purpose: Despite the significant role of varicocele in the pathogenesis of male infertility, the impact of varicocele repair (VR) on conventional semen parameters remains controversial. Only a few systematic reviews and meta-analyses (SRMAs) have evaluated the impact of VR on sperm concentration, total motility, and progressive motility, mostly using a before-after analytic approach. No SRMA to date has evaluated the change in conventional semen parameters after VR compared to untreated controls. This study aimed to evaluate the effect of VR on conventional semen parameters in infertile patients with clinical varicocele compared to untreated controls.
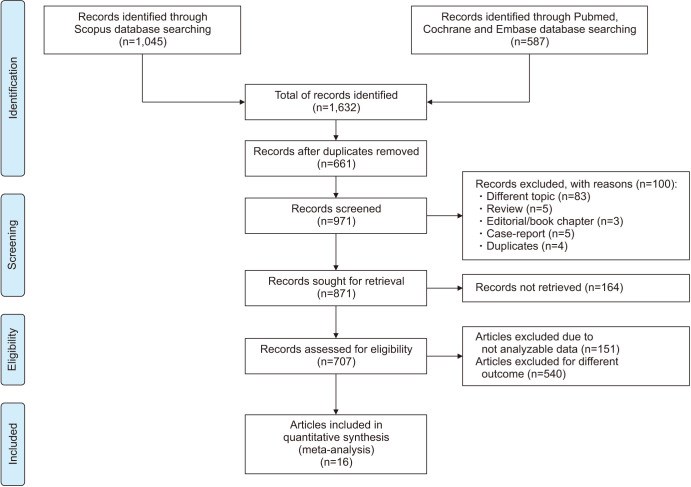
Materials and methods: A literature search was performed using Scopus, PubMed, Embase, and Cochrane databases following the Population Intervention Comparison Outcome (PICOS) model (Population: infertile patients with clinical varicocele; Intervention: VR [any technique]; Comparison: infertile patients with clinical varicocele that were untreated; Outcome: sperm concentration, sperm total count, progressive sperm motility, total sperm motility, sperm morphology, and semen volume; Study type: randomized controlled trials and observational studies).
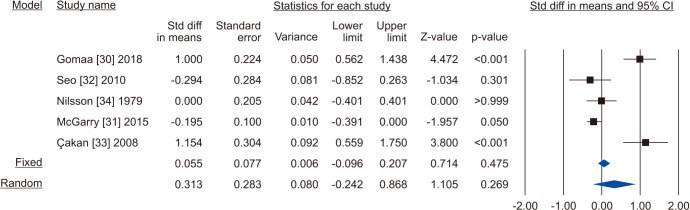
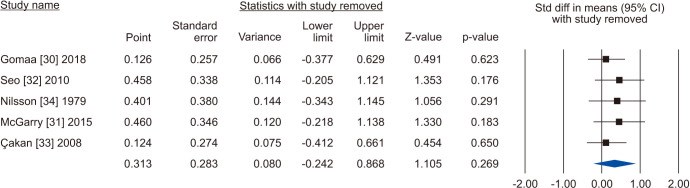
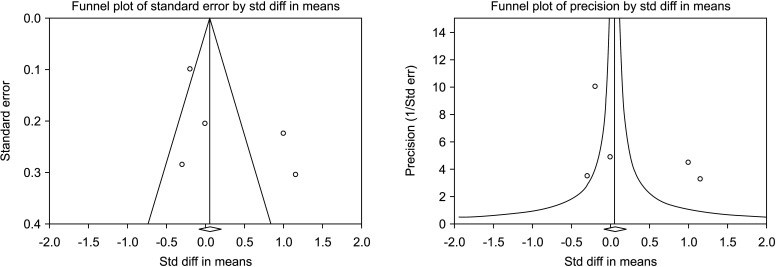
Results: A total of 1,632 abstracts were initially assessed for eligibility. Sixteen studies were finally included with a total of 2,420 infertile men with clinical varicocele (1,424 patients treated with VR vs. 996 untreated controls). The analysis showed significantly improved post-operative semen parameters in patients compared to controls with regards to sperm concentration (standardized mean difference [SMD] 1.739; 95% CI 1.129 to 2.349; p<0.001; I²=97.6%), total sperm count (SMD 1.894; 95% CI 0.566 to 3.222; p<0.05; I²=97.8%), progressive sperm motility (SMD 3.301; 95% CI 2.164 to 4.437; p<0.01; I²=98.5%), total sperm motility (SMD 0.887; 95% CI 0.036 to 1.738; p=0.04; I²=97.3%) and normal sperm morphology (SMD 1.673; 95% CI 0.876 to 2.470; p<0.05; I²=98.5%). All the outcomes showed a high inter-study heterogeneity, but the sensitivity analysis showed that no study was sensitive enough to change these results. Publication bias was present only in the analysis of the sperm concentration and progressive motility. No significant difference was found for the semen volume (SMD 0.313; 95% CI -0.242 to 0.868; I²=89.7%).
Conclusions: This study provides a high level of evidence in favor of a positive effect of VR to improve conventional semen parameters in infertile men with clinical varicocele. To the best of our knowledge, this is the first SRMA to compare changes in conventional semen parameters after VR with changes in parameters of a control group over the same period. This is in contrast to other SRMAs which have compared semen parameters before and after VR, without reference to a control group. Our findings strengthen the available evidence and have a potential to upgrade professional societies' practice recommendations favoring VR to improve conventional semen parameters in infertile men.
Keywords: Male infertility; Semen; Varicocele.
Conflict of interest statement
The authors have nothing to disclose.
Figures
Similar articles
Agarwal A, Cannarella R, Saleh R, Harraz AM, Kandil H, Salvio G, Boitrelle F, Kuroda S, Farkouh A, Rambhatla A, Zini A, Colpi G, Gül M, Kavoussi P, Hamoda TAA, Ko E, Calik G, Toprak T, Pinggera GM, Park HJ, Ghayda RA, Minhas S, Busetto GM, Bakırcıoğlu ME, Kadioglu A, Chung E, Russo GI, Calogero AE, Ambar RF, Jayasena CN, Shah R.World J Mens Health. 2023 Jan;41(1):14-48. doi: 10.5534/wjmh.220067. Epub 2022 Sep 7.PMID: 36102104 Free PMC article.
Fallara G, Capogrosso P, Pozzi E, Belladelli F, Corsini C, Boeri L, Candela L, Schifano N, Dehò F, Castiglione F, Muneer A, Montorsi F, Salonia A.Eur Urol Focus. 2023 Jan;9(1):154-161. doi: 10.1016/j.euf.2022.08.014. Epub 2022 Sep 20.PMID: 36151030 Review.
Nomograms for predicting changes in semen parameters in infertile men after varicocele repair.
Samplaski MK, Yu C, Kattan MW, Lo KC, Grober ED, Zini A, Lau S, Jarvi KA.Fertil Steril. 2014 Jul;102(1):68-74. doi: 10.1016/j.fertnstert.2014.03.046. Epub 2014 May 10.PMID: 24825425
Crider K, Williams J, Qi YP, Gutman J, Yeung L, Mai C, Finkelstain J, Mehta S, Pons-Duran C, Menéndez C, Moraleda C, Rogers L, Daniels K, Green P.Cochrane Database Syst Rev. 2022 Feb 1;2(2022):CD014217. doi: 10.1002/14651858.CD014217.PMID: 36321557 Free PMC article.
Cui D, Han G, Shang Y, Liu C, Xia L, Li L, Yi S.Clin Chim Acta. 2015 Apr 15;444:29-36. doi: 10.1016/j.cca.2015.01.033. Epub 2015 Feb 7.PMID: 25659295 Review.
Cited by
Mahdi M, Majzoub A, Elbardisi H, Arafa M, Khalafalla K, Al Said S, El Ansari W.Arab J Urol. 2023 May 9;21(3):190-197. doi: 10.1080/2090598X.2023.2206336. eCollection 2023.PMID: 37521450 Free PMC article.
Crafa A, Calogero AE, Cannarella R, Condorelli RA, Aversa A, La Vignera S.J Clin Med. 2023 Apr 27;12(9):3152. doi: 10.3390/jcm12093152.PMID: 37176596 Free PMC article.
KMEL References
References
-
- Thonneau P, Marchand S, Tallec A, Ferial ML, Ducot B, Lansac J, et al. Incidence and main causes of infertility in a resident population (1,850,000) of three French regions (1988-1989) Hum Reprod. 1991;6:811–816. - PubMed
-
- Odisho AY, Nangia AK, Katz PP, Smith JF. Temporal and geospatial trends in male factor infertility with assisted reproductive technology in the United States from 1999-2010. Fertil Steril. 2014;102:469–475. - PubMed
-
- Freeman S, Bertolotto M, Richenberg J, Belfield J, Dogra V, Huang DY, et al. members of the ESUR-SPIWG WG. Ultrasound evaluation of varicoceles: guidelines and recommendations of the European Society of Urogenital Radiology Scrotal and Penile Imaging Working Group (ESUR-SPIWG) for detection, classification, and grading. Eur Radiol. 2020;30:11–25. - PubMed
-
- Damsgaard J, Joensen UN, Carlsen E, Erenpreiss J, Blomberg Jensen M, Matulevicius V, et al. Varicocele is associated with impaired semen quality and reproductive hormone levels: a study of 7035 healthy young men from six European countries. Eur Urol. 2016;70:1019–1029. - PubMed
-
- Gorelick JI, Goldstein M. Loss of fertility in men with varicocele. Fertil Steril. 1993;59:613–616. - PubMed
-
- Jarow JP, Coburn M, Sigman M. Incidence of varicoceles in men with primary and secondary infertility. Urology. 1996;47:73–76. - PubMed
-
- World Health Organization. The influence of varicocele on parameters of fertility in a large group of men presenting to infertility clinics. Fertil Steril. 1992;57:1289–1293. - PubMed
-
- Schlegel PN, Sigman M, Collura B, De Jonge CJ, Eisenberg ML, Lamb DJ, et al. Diagnosis and treatment of infertility in men: AUA/ASRM guideline part I. Fertil Steril. 2021;115:54–61. - PubMed
-
- Minhas S, Bettocchi C, Boeri L, Capogrosso P, Carvalho J, Cilesiz NC, et al. EAU Working Group on Male Sexual and Reproductive Health. European Association of Urology guidelines on male sexual and reproductive health: 2021 update on male infertility. Eur Urol. 2021;80:603–620. - PubMed
-
- Baazeem A, Belzile E, Ciampi A, Dohle G, Jarvi K, Salonia A, et al. Varicocele and male factor infertility treatment: a new meta-analysis and review of the role of varicocele repair. Eur Urol. 2011;60:796–808. - PubMed
-
- Agarwal A, Deepinder F, Cocuzza M, Agarwal R, Short RA, Sabanegh E, et al. Efficacy of varicocelectomy in improving semen parameters: new meta-analytical approach. Urology. 2007;70:532–538. - PubMed
-
- Colpi GM, Francavilla S, Haidl G, Link K, Behre HM, Goulis DG, et al. European Academy of Andrology guideline management of oligo-astheno-teratozoospermia. Andrology. 2018;6:513–524. - PubMed
-
- Marmar JL, Agarwal A, Prabakaran S, Agarwal R, Short RA, Benoff S, et al. Reassessing the value of varicocelectomy as a treatment for male subfertility with a new meta-analysis. Fertil Steril. 2007;88:639–648. - PubMed
-
- Kroese AC, de Lange NM, Collins J, Evers JL. Surgery or embolization for varicoceles in subfertile men. Cochrane Database Syst Rev. 2012;10:CD000479. - PubMed
-
- Shah R, Agarwal A, Kavoussi P, Rambhatla A, Saleh R, Cannarella R, et al. Consensus and diversity in the management of varicocele for male infertility: results of a global practice survey and comparison with guidelines and recommendations. World J Mens Health. 2022 doi: 10.5534/wjmh.220048. [Epub] - DOI - PMC - PubMed
-
- Schauer I, Madersbacher S, Jost R, Hübner WA, Imhof M. The impact of varicocelectomy on sperm parameters: a meta-analysis. J Urol. 2012;187:1540–1547. - PubMed
-
- Asafu-Adjei D, Judge C, Deibert CM, Li G, Stember D, Stahl PJ. Systematic review of the impact of varicocele grade on response to surgical management. J Urol. 2020;203:48–56. - PubMed
-
- Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA. 2000;283:2008–2012. - PubMed
-
- Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;350:g7647. Erratum in: BMJ 2016;354:i4086. - PubMed
-
- Murray J, Farrington DP, Eisner MP. Drawing conclusions about causes from systematic reviews of risk factors: the Cambridge Quality Checklists. J Exp Criminol. 2009;5:1–23.
-
- Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. - PubMed
-
- Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12. - PubMed
-
- Huedo-Medina TB, Sánchez-Meca J, Marín-Martínez F, Botella J. Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol Methods. 2006;11:193–206. - PubMed
-
- Andrade C. Mean difference, standardized mean difference (SMD), and their use in meta-analysis: as simple as it gets. J Clin Psychiatry. 2020;81:20f13681 - PubMed
-
- Duval S, Tweedie R. A nonparametric “trim and fill” method of accounting for publication bias in meta-analysis. J Am Stat Assoc. 2000;95:89–98.
-
- Gomaa MD, Motawaa MA, Al-Nashar AM, El-Sakka AI. Impact of subinguinal varicocelectomy on serum testosterone to estradiol ratio in male patients with infertility. Urology. 2018;117:70–77. - PubMed
-
- McGarry P, Alrabeeah K, Jarvi K, Zini A. Is varicocelectomy beneficial in men previously deemed subfertile but with normal semen parameters based on the new guidelines? A retrospective study. Urology. 2015;85:357–362. - PubMed
-
- Seo JT, Kim KT, Moon MH, Kim WT. The significance of microsurgical varicocelectomy in the treatment of subclinical varicocele. Fertil Steril. 2010;93:1907–1910. - PubMed
-
- Çakan M, Bakirtas H, Aldemir M, Demirel F, Altug U. Results of varicocelectomy in patients with isolated teratozoospermia. Urol Int. 2008;80:172–176. - PubMed
-
- Nilsson S, Edvinsson A, Nilsson B. Improvement of semen and pregnancy rate after ligation and division of the internal spermatic vein: fact or fiction? Br J Urol. 1979;51:591–596. - PubMed
-
- Turgut H. The effect of varicocelectomy on the pregnancy rate in patients with severe oligospermia. Niger J Clin Pract. 2020;23:1744–1747. - PubMed
-
- Gokce MI, Gülpınar O, Süer E, Mermerkaya M, Aydos K, Yaman O. Effect of performing varicocelectomy before intracytoplasmic sperm injection on clinical outcomes in non-azoospermic males. Int Urol Nephrol. 2013;45:367–372. - PubMed
-
- Mansour Ghanaie M, Asgari SA, Dadrass N, Allahkhah A, Iran-Pour E, Safarinejad MR. Effects of varicocele repair on spontaneous first trimester miscarriage: a randomized clinical trial. Urol J. 2012;9:505–513. - PubMed
-
- Abdel-Meguid TA, Al-Sayyad A, Tayib A, Farsi HM. Does varicocele repair improve male infertility? An evidence-based perspective from a randomized, controlled trial. Eur Urol. 2011;59:455–461. - PubMed
-
- Di Bisceglie C, Bertagna A, Baldi M, Lanfranco F, Tagliabue M, Gazzera C, et al. Varicocele sclerotherapy improves serum inhibin B levels and seminal parameters. Int J Androl. 2007;30:531–536. - PubMed
-
- Di Bisceglie C, Fornengo R, Grosso M, Gazzera C, Mancini A, Andriani B, et al. Follow-up of varicocele treated with percutaneous retrograde sclerotherapy: technical, clinical and seminal aspects. J Endocrinol Invest. 2003;26:1059–1064. - PubMed
-
- Grasso M, Lania C, Castelli M, Galli L, Franzoso F, Rigatti P. Low-grade left varicocele in patients over 30 years old: the effect of spermatic vein ligation on fertility. BJU Int. 2000;85:305–307. - PubMed
-
- Okuyama A, Fujisue H, Matsui T, Doi Y, Takeyama M, Nakamura N, et al. Surgical repair of varicocele: effective treatment for subfertile men in a controlled study. Eur Urol. 1988;14:298–300. - PubMed
-
- Ketabchi AA, Salajegheh S. The effects of acupuncture treatment in infertile patients with clinical varicocele. Nephrourol Mon. 2018;10:e65451
-
- Schlegel PN, Sigman M, Collura B, De Jonge CJ, Eisenberg ML, Lamb DJ, et al. Diagnosis and treatment of infertility in men: AUA/ASRM guideline part II. J Urol. 2021;205:44–51. - PubMed
-
- Silber SJ. The varicocele dilemma. Hum Reprod Update. 2001;7:70–77. - PubMed
-
- Baker HW, Kovacs GT. Spontaneous improvement in semen quality: regression towards the mean. Int J Androl. 1985;8:421–426. - PubMed
-
- Kroese ACJ, de Lange NM, Collins J, Evers JLH, Marjoribanks J. Surgery or embolization for varicoceles in subfertile men: summary of a Cochrane review. Fertil Steril. 2014;102:1553–1555.
-
- Hinkelmann K, Kempthorne O. Design and analysis of experiments. 2nd ed. Vol. 1, Introduction to experimental design. Hoboken (NJ): Wiley; 2008.
-
- Teoli D, Sanvictores T, An J. In: StatPearls. Abai B, Abu-Ghosh A, Acharya AB, Acharya U, Adhia SG, Sedeh PA, editors. Treasure Island (FL): StatPearls Publishing; 2022. SWOT analysis. - PubMed