Utilization of dental services among low and middle income pregnant, post-partum and six-month post-partum women
Affiliations
Affiliations
- Division of Dental Public Health, Department of Developmental and Preventive Sciences, Faculty of Dentistry, Kuwait University, 13110, Kuwait City, Kuwait. drjaganb@gmail.com.
- Resident, Dental Public Health, Department of Preventive and Restorative Dental Sciences, School of Dentistry, University of California San Francisco, 707 Parnassus Avenue, San Francisco, CA, 94143, USA.
Abstract
Background: This study aims to explore the difference in the utilization pattern of dental services among pregnant, post-partum and six-month post-partum women.
Methods: This cross-sectional questionnaire survey was performed at two maternity and child care hospitals in India that primarily cater to middle and low income communities. Data were collected from 3 groups: 1) pregnant women in their first trimester; 2) post-partum women (< 48 h after delivery); and 3) six-month post-partum women. The primary outcome of interest was dental service utilization during pregnancy. Self-perceived oral health (SPOH) was calculated based on the four global dimensions- knowledge, function, quality of life and social. Multiple logistic regression analysis was carried out to assess the effect of each independent variable after adjustment for the effect of all other variables in the model.
Results: Responses of 450 (150 pregnant, 150 post-partum and 150 six-month post-partum) women were analyzed (response rate = 72%). Significant differences in the dental attendance pattern was observed between the study groups (p < 0.01). Dental attendance among pregnant and six-month post-partum women were 60 and 75%, respectively, however, only about 15% of the post-partum women reported to have sought dental care within the 6 months prior to the study. Post-partum women had the highest SPOH scores, indicating poor self-perceived oral health, followed by pregnant and then six-month post-partum women, which was statistically significant (p < 0.05). A significantly higher percentage of post-partum women reported to have poor oral and general health, as compared to both, pregnant and six-month post-partum women (p < 0.01). Higher percentage of women reporting 'good' oral and general health had sought dental care compared with others (p < 0.01). After adjusting for all the other variables in the model, women with lower levels of education (ORa = 1.42; 95% CI: 1.01-2.00), women with poor self-perceived oral health (ORa = 1.08; 95% CI: 1.02-1.14) and post-partum women (ORa = 0.15; 95% CI: 0.09-0.24) were found to be less likely to seek regular dental care.
Conclusion: Pattern of dental service utilization among women in this population varied according to their pregnancy status, level of education and self-perceived oral health.
Conflict of interest statement
The authors declare that they have no competing interests.
Figures
Similar articles
An official website of the United States government
Here's how you know
Access keysNCBI HomepageMyNCBI HomepageMain ContentMain Navigation
Search:0 results are available, use up and down arrow keys to navigate.Search
SaveEmail
Send to
Display options
Abstract PubMed PMID
full text links
actions
Cite
Collections
share
page navigation
- Title & authors
- Abstract
- Conflict of interest statement
- Figures
- Similar articles
- Cited by
- References
- MeSH terms
- LinkOut - more resources
Title & authors Abstract Conflict of interest statement Figures Similar articles Cited by References MeSH terms LinkOut - more resources
BMC Oral Health
. 2020 Apr 20;20(1):120.
doi: 10.1186/s12903-020-01076-9.
Utilization of dental services among low and middle income pregnant, post-partum and six-month post-partum women
Jagan Kumar Baskaradoss 1, Amrita Geevarghese 2
Affiliations expand
- PMID: 32312257
- PMCID: PMC7171727
- DOI: 10.1186/s12903-020-01076-9
Free PMC article
Abstract
Background: This study aims to explore the difference in the utilization pattern of dental services among pregnant, post-partum and six-month post-partum women.
Methods: This cross-sectional questionnaire survey was performed at two maternity and child care hospitals in India that primarily cater to middle and low income communities. Data were collected from 3 groups: 1) pregnant women in their first trimester; 2) post-partum women (< 48 h after delivery); and 3) six-month post-partum women. The primary outcome of interest was dental service utilization during pregnancy. Self-perceived oral health (SPOH) was calculated based on the four global dimensions- knowledge, function, quality of life and social. Multiple logistic regression analysis was carried out to assess the effect of each independent variable after adjustment for the effect of all other variables in the model.
Results: Responses of 450 (150 pregnant, 150 post-partum and 150 six-month post-partum) women were analyzed (response rate = 72%). Significant differences in the dental attendance pattern was observed between the study groups (p < 0.01). Dental attendance among pregnant and six-month post-partum women were 60 and 75%, respectively, however, only about 15% of the post-partum women reported to have sought dental care within the 6 months prior to the study. Post-partum women had the highest SPOH scores, indicating poor self-perceived oral health, followed by pregnant and then six-month post-partum women, which was statistically significant (p < 0.05). A significantly higher percentage of post-partum women reported to have poor oral and general health, as compared to both, pregnant and six-month post-partum women (p < 0.01). Higher percentage of women reporting 'good' oral and general health had sought dental care compared with others (p < 0.01). After adjusting for all the other variables in the model, women with lower levels of education (ORa = 1.42; 95% CI: 1.01-2.00), women with poor self-perceived oral health (ORa = 1.08; 95% CI: 1.02-1.14) and post-partum women (ORa = 0.15; 95% CI: 0.09-0.24) were found to be less likely to seek regular dental care.
Conclusion: Pattern of dental service utilization among women in this population varied according to their pregnancy status, level of education and self-perceived oral health.
Conflict of interest statement
The authors declare that they have no competing interests.
Figures

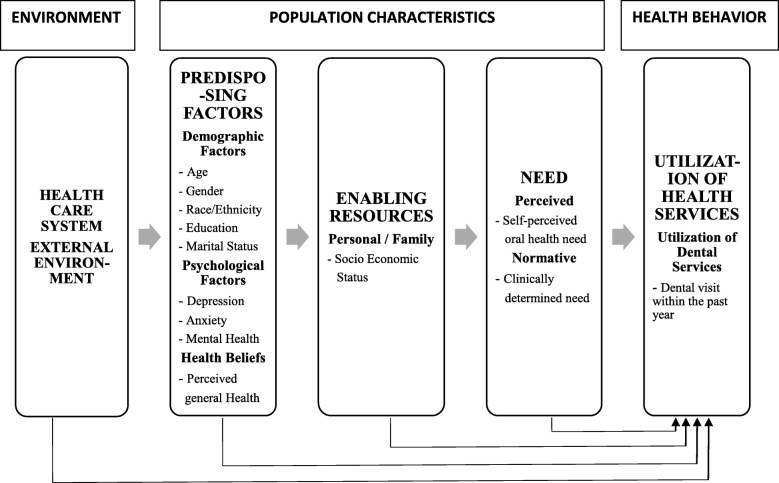
Fig. 1
Andersen’s emerging behavioral model of…
Similar articles
Utilization of dental services and associated factors among preschool children in China.
Gao X, Ding M, Xu M, Wu H, Zhang C, Wang X, Feng X, Tai B, Hu D, Lin H, Wang B, Zheng S, Liu X, Rong W, Wang W, Wang C, Si Y.BMC Oral Health. 2020 Jan 8;20(1):9. doi: 10.1186/s12903-019-0996-x.PMID: 31914978 Free PMC article.
Xu M, Cheng M, Gao X, Wu H, Ding M, Zhang C, Wang X, Feng X, Tai B, Hu D, Lin H, Wang B, Wang C, Zheng S, Liu X, Rong W, Wang W, Xu T, Si Y.Community Dent Oral Epidemiol. 2020 Feb;48(1):32-41. doi: 10.1111/cdoe.12497. Epub 2019 Oct 16.PMID: 31621099
Chawla RM, Shetiya SH, Agarwal DR, Mitra P, Bomble NA, Narayana DS.J Contemp Dent Pract. 2017 May 1;18(5):371-377. doi: 10.5005/jp-journals-10024-2049.PMID: 28512275
The oral health of Indigenous pregnant women: A mixed-methods systematic review.
Kong AC, Ramjan L, Sousa MS, Gwynne K, Goulding J, Jones N, Srinivas R, Rambaldini B, Moir R, George A.Women Birth. 2020 Jul;33(4):311-322. doi: 10.1016/j.wombi.2019.08.007. Epub 2019 Sep 7.PMID: 31501053 Review.
Access and use of dental services by pregnant women: an integrative literature review.
Silva CCD, Savian CM, Prevedello BP, Zamberlan C, Dalpian DM, Santos BZD.Cien Saude Colet. 2020 Mar;25(3):827-835. doi: 10.1590/1413-81232020253.01192018. Epub 2018 Jul 7.PMID: 32159653 Review. English, Portuguese.
Cited by
Talukdar R, Barman D, Thakkar V, Kanungo S.Health Promot Perspect. 2022 Dec 31;12(4):325-335. doi: 10.34172/hpp.2022.42. eCollection 2022.PMID: 36852206 Free PMC article.
Gaspar-Damaso N, Ladera-Castañeda M, Córdova-Limaylla N, Briceño-Vergel G, Cervantes-Ganoza L, Nicho-Valladares M, Cornejo-Pinto A, Echavarría-Gálvez A, Cayo-Rojas C.Int J Environ Res Public Health. 2023 Jan 19;20(3):1881. doi: 10.3390/ijerph20031881.PMID: 36767256 Free PMC article.
KMEL References
References
-
- Baskaradoss JK, Geevarghese A, Kutty VR. Maternal periodontal status and preterm delivery: a hospital based case-control study. J Periodontal Res. 2011;46(5):542–549. - PubMed
-
- Ide M, Papapanou PN. Epidemiology of association between maternal periodontal disease and adverse pregnancy outcomes--systematic review. J Clin Periodontol. 2013;40(Suppl 14):S181–S194. - PubMed
-
- von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, Initiative S. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495–1499. doi: 10.1016/j.ijsu.2014.07.013. - DOI - PubMed
-
- International Institute for Population Sciences (IIPS) and University of Kerala: National Family Health Survey (NFHS-2), India, 1998–99: Kerala. Bombay 2001.
-
- Ekback G, Astrom AN, Klock K, Ordell S, Unell L. Self-perceived oral health among 19-year-olds in two Swedish counties. Swed Dent J. 2008;32(2):83–93. - PubMed