Prevalence of antimicrobial resistance in Gram-negative clinical isolates from a major secondary hospital in Kuwait: a retrospective descriptive study
Affiliations
Affiliations
- DVM, PhD, Department of Epidemiology & Biostatistics, Faculty of Public Health, Kuwait University, Hawalli, postal code 13060, Kuwait.
- MD, PhD, Microbiology Unit, Department of Laboratories, Farwaniya Hospital, Farwaniya, postal code 85000, Kuwait, Department of Microbiology, Faculty of Medicine, Kuwait University, Jabriya, postal code 85000, Kuwait.
- MD, PhD, Microbiology Unit, Department of Laboratories, Farwaniya Hospital, Farwaniya, postal code 85000, Kuwait.
Abstract
Introduction: Building an antimicrobial resistance (AMR) surveillance system in a country requires analysis of available data on AMR in clinical isolates. This study's objective was to determine the AMR prevalence of Gram-negative bacterial (GNB) isolates cultured from clinical specimens at a major general hospital in Kuwait.
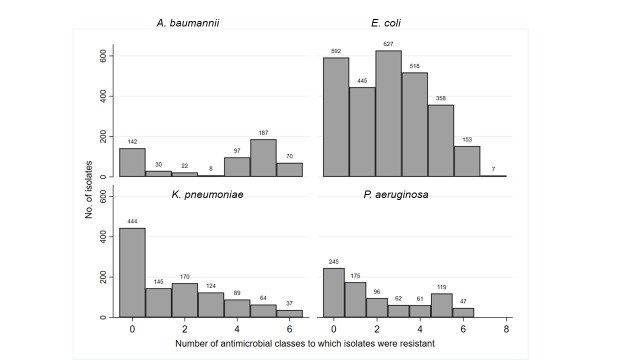
Methods: A retrospective descriptive study was conducted on AMR profiles of GNB clinical isolates (n=5290) between January and December 2018. Data were extracted from the laboratory information system in the hospital. The GNB organisms (i.e., Escherichia coli, Klebsiella pneumoniae, Pseudomonas aeruginosa, and Acinetobacter baumannii) were isolated from five main locations at the hospital (i.e., intensive care units [ICUs], surgical wards, medical wards, pediatric wards, and outpatient polyclinics).
Results: Overall, high AMR prevalence (>50%) against ampicillin, cefuroxime, cefotaxime, ceftazidime, ciprofloxacin, and trimethoprim/sulfamethoxazole, were observed across the GNB organisms. However, low resistance prevalence (<10%) were observed against amikacin, ertapenem, meropenem, and piperacillin/tazobactam. In general, AMR prevalence in E. coli isolates from ICU, medical and surgical wards was significantly (p<0.05) higher compared to other locations, whereas, AMR prevalence in P. aeruginosa isolates from pediatric ward was higher (p<0.05) compared to other locations. The overall multidrug resistance (MDR) prevalence was 38.7% (95% CI: 37.4-40.0). The highest MDR prevalence was among E. coli isolates from respiratory specimens (48%); wounds, bones, or other tissues (47.7%); and body fluids (47.1%). Similarly, MDR prevalence in K. pneumoniae, P. aeruginosa, and A. baumannii isolated from respiratory specimens was significantly (p<0.05) higher compared to other specimen types. The most frequent MDR phenotypes in the four GNB organisms and across the different specimen types included three antimicrobial drug classes: penicillins, cephalosporins, and fluroquinolones.
Conclusions: Our findings demonstrate high AMR prevalence among common Gram-negative bacteria at this major hospital. Monitoring data on antimicrobial susceptibility of common bacterial organisms is critical for assessing trends in AMR at hospitals and for informing policy decisions.
Keywords: Bacterial resistance; Middle East; critical care; hospital-acquired infections; multidrug resistance; public health.
GERMS.
Conflict of interest statement
Conflicts of interest: All authors – none to declare.
Figures
Similar articles
Uc-Cachón AH, Gracida-Osorno C, Luna-Chi IG, Jiménez-Guillermo JG, Molina-Salinas GM.Medicina (Kaunas). 2019 Sep 13;55(9):588. doi: 10.3390/medicina55090588.PMID: 31540314 Free PMC article.
Donkor ES, Muhsen K, Johnson SAM, Kotey FCN, Dayie NTKD, Tetteh-Quarcoo PB, Tette EMA, Osei MM, Egyir B, Nii-Trebi NI, Owusu-Okyere G, Owusu-Ofori A, Amir Y, Perlman S, Lopes PH, Mfodwo A, Gordon NC, Gresham L, Smolinski M, Cohen D.Antibiotics (Basel). 2023 Jan 27;12(2):255. doi: 10.3390/antibiotics12020255.PMID: 36830166 Free PMC article.
Zhanel GG, DeCorby M, Laing N, Weshnoweski B, Vashisht R, Tailor F, Nichol KA, Wierzbowski A, Baudry PJ, Karlowsky JA, Lagacé-Wiens P, Walkty A, McCracken M, Mulvey MR, Johnson J; Canadian Antimicrobial Resistance Alliance (CARA); Hoban DJ.Antimicrob Agents Chemother. 2008 Apr;52(4):1430-7. doi: 10.1128/AAC.01538-07. Epub 2008 Feb 19.PMID: 18285482 Free PMC article.
Al Dabbagh M, Alghounaim M, Almaghrabi RH, Dbaibo G, Ghatasheh G, Ibrahim HM, Aziz MA, Hassanien A, Mohamed N.Infect Dis Ther. 2023 May;12(5):1217-1235. doi: 10.1007/s40121-023-00799-w. Epub 2023 Apr 18.PMID: 37071349 Free PMC article. Review.
Phu DH, Wongtawan T, Truong DB, Van Cuong N, Carrique-Mas J, Thomrongsuwannakij T.One Health. 2022 Nov 19;15:100465. doi: 10.1016/j.onehlt.2022.100465. eCollection 2022 Dec.PMID: 36561710 Free PMC article. Review.
Cited by
Mwansa TN, Kamvuma K, Mulemena JA, Phiri CN, Chanda W.PLOS Glob Public Health. 2022 Sep 14;2(9):e0000623. doi: 10.1371/journal.pgph.0000623. eCollection 2022.PMID: 36962542 Free PMC article.
Ponyon J, Kerdsin A, Preeprem T, Ungcharoen R.Trop Med Infect Dis. 2022 Oct 23;7(11):328. doi: 10.3390/tropicalmed7110328.PMID: 36355871 Free PMC article.