Photobiomodulation for Managing "Dry Socket": A Randomised Controlled Trial
Affiliations
Affiliations
- Department of Preventive Dental Sciences, College of Dentistry, Princess Nourah Bint Abdulrahman University, Riyadh, Saudi Arabia.
- Department of General Dental Practice, Kuwait University, Safat, Kuwait.
- Department of Preventive Dental Sciences, College of Dentistry, King Saud Bin Abdulaziz University, Riyadh, Saudi Arabia; King Abdullah International Medical Research Center, Riyadh, Saudi Arabia.
- Department of Oral Medicine and Radiology, Sharavathi Dental College and Hospital, Shivamogga, Karnataka, India; Department of Oral Medicine and Radiology, Faculty of Dentistry, Levy Mwanawasa Medical University, Ministry of Health, Lusaka, Zambia.
- Department of Preventive Dental Sciences, College of Dentistry, Princess Nourah Bint Abdulrahman University, Riyadh, Saudi Arabia. Electronic address: MSbinshabaib@pnu.edu.sa.
Abstract
Objective: There are no studies that have evaluated the effect of Alveogyl with and without adjunct photobiomodulation therapy (PBMT) in reducing self-rated post-operative pain (SPP) in patients with alveolar osteitis (AO; dry socket). The aim of the present randomised controlled trial was to assess the effectiveness of Alveogyl with and without PBMT for the management of SPP in patients with AO.
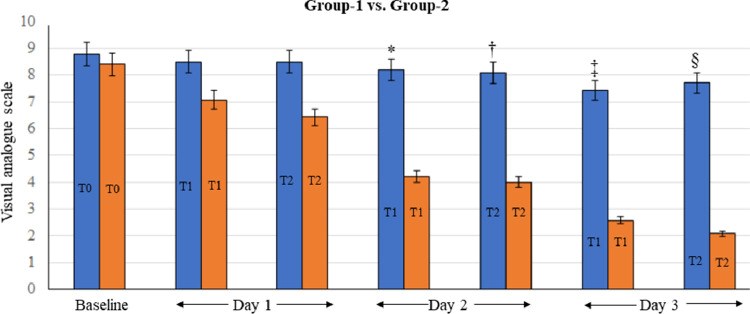
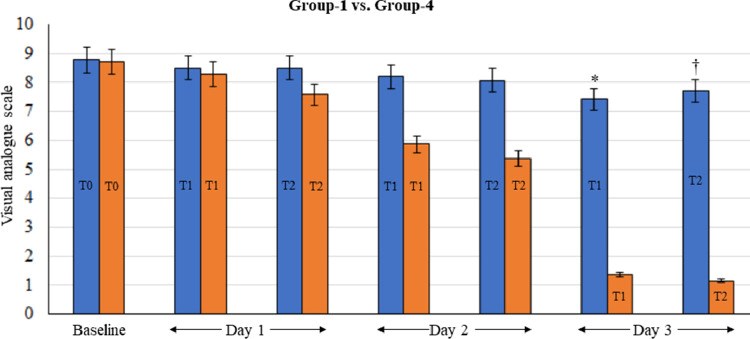
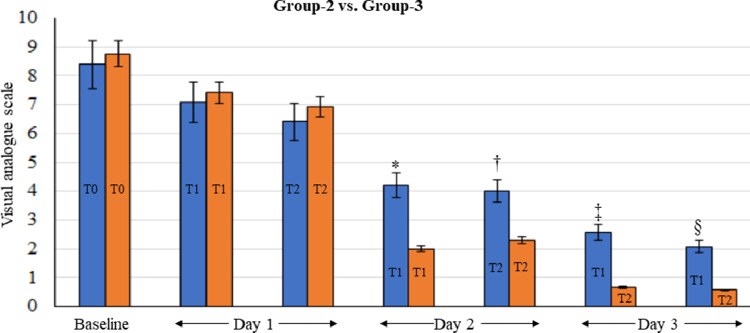
Methods: Adult nonsmokers with diagnosed AO were included. Patients were randomly divided into 4 groups. In Group 1, patients underwent mechanical curettage (MC) with copious normal saline irrigation. In Group 2, patients underwent MC + Alveogyl dressings in extraction sites which were changed every 48 hours until cessation of pain. In Group 3, patients underwent MC + Alveogyl followed by PBMT using a 660-nm indium-gallium-aluminum-phosphide diode laser. In Group 4, patients were treated solely with PBMT. The visual analogue scale was used up to 3 postoperative days to assess SPP up to 3 days at 6- (T0) and 12-hour (T1) intervals. Statistical analyses were performed using the analysis of variance and Bonferroni post hoc adjustment tests. Correlation between SPP scores and age, sex, and eruption status of teeth was assessed using logistic regression models. P values <.01 were nominated as being statistically significant.
Results: In all, 14, 13, 14, and 14 individuals with AO were included in groups 1, 2, 3 and 4, respectively. All patients had undergone extraction of mandibular third molars. At baseline and on day 1, there was no difference in SPP in all groups. On days 2 and 3, mean visual analogue scale (VAS) scores at T1 (P < .01) and T2 (P < .01) intervals were significantly high in Group 2 compared with Group 3. On days 2 and 3, mean VAS scores at T1 (P < .01) and T2 (P < .01) intervals were significantly high in Group 4 compared with Group 3. There was no difference in SPP in groups 3 and 4 on day 3 at T0 and T1 intervals.
Conclusions: PBMT following MC and Alveogyl dressing is more efficient in reducing SPP compared with MC with or without Alveogyl dressing in patients with AO.
Keywords: Alveogyl; Alveolar osteitis; Pain; Photobiomodulation; Visual analogue scale.
Conflict of interest statement
Conflict of interest None disclosed.
Figures
Similar articles
Tolstunov L.Br Dent J. 2012 Dec;213(12):597-601. doi: 10.1038/sj.bdj.2012.1134.PMID: 23257808
Nejat AH, Eshghpour M, Danaeifar N, Abrishami M, Vahdatinia F, Fekrazad R.Photochem Photobiol. 2021 Sep;97(5):1129-1135. doi: 10.1111/php.13457. Epub 2021 Jun 17.PMID: 34048061 Clinical Trial.
Sun YQ, Sun R, Zhao JH.BMC Oral Health. 2022 Oct 18;22(1):448. doi: 10.1186/s12903-022-02468-9.PMID: 36258229 Free PMC article.
Shafaee H, Bardideh E, Nazari MS, Asadi R, Shahidi B, Rangrazi A.Photodiagnosis Photodyn Ther. 2020 Dec;32:102000. doi: 10.1016/j.pdpdt.2020.102000. Epub 2020 Sep 9.PMID: 32919077 Review.
Local interventions for the management of alveolar osteitis (dry socket).
Daly BJ, Sharif MO, Jones K, Worthington HV, Beattie A.Cochrane Database Syst Rev. 2022 Sep 26;9(9):CD006968. doi: 10.1002/14651858.CD006968.pub3.PMID: 36156769 Review.
KMEL References
References
-
- Tolstunov L. Influence of immediate post-extraction socket irrigation on development of alveolar osteitis after mandibular third molar removal: a prospective split-mouth study, preliminary report. Br Dent J. 2012;213:597–601. - PubMed
-
- Adeyemo WL, Ladeinde AL, Ogunlewe MO. Clinical evaluation of post-extraction site wound healing. J Contemp Dent Pract. 2006;7:40–49. - PubMed
-
- Blum IR. Contemporary views on dry socket (alveolar osteitis): a clinical appraisal of standardization, aetiopathogenesis and management: a critical review. Int J Oral Maxillofac Surg. 2002;31:309–317. - PubMed
-
- Blondeau F, Daniel NG. Extraction of impacted mandibular third molars: postoperative complications and their risk factors. J Can Dent Assoc. 2007;73:325. - PubMed
-
- Rakhshan V. Common risk factors of dry socket (alveolitis osteitis) following dental extraction: A brief narrative review. J Stomatol Oral Maxillofac Surg. 2018;119:407–411. - PubMed
-
- Catellani JE, Harvey S, Erickson SH, Cherkin D. Effect of oral contraceptive cycle on dry socket (localized alveolar osteitis) J Am Dent Assoc. 1980;101:777–780. - PubMed
-
- Oginni FO. Dry socket: a prospective study of prevalent risk factors in a Nigerian population. J Oral Maxillofac Surg. 2008;66:2290–2295. - PubMed
-
- Chaurasia NK, Upadhyaya C, Dixit S. Comparative study to determine the efficacy of zinc oxide eugenol and alveogyl in treatment of dry socket. Kathmandu Univ Med J (KUMJ) 2017;15:203–206. - PubMed
-
- Jesudasan JS, Wahab PU, Sekhar MR. Effectiveness of 0.2% chlorhexidine gel and a eugenol-based paste on postoperative alveolar osteitis in patients having third molars extracted: a randomised controlled clinical trial. Br J Oral Maxillofac Surg. 2015;53:826–830. - PubMed
-
- Haraji A, Rakhshan V, Khamverdi N, Alishahi HK. Effects of intra-alveolar placement of 0.2% chlorhexidine bioadhesive gel on dry socket incidence and postsurgical pain: a double-blind split-mouth randomized controlled clinical trial. J Orofac Pain. 2013;27:256–262. - PubMed
-
- Dubovina D, Mihailović B, Bukumirić Z, et al. The use of hyaluronic and aminocaproic acid in the treatment of alveolar osteitis. Vojnosanit Pregl. 2016;73:1010–1015. - PubMed
-
- Shafaee H, Bardideh E, Nazari MS, Asadi R, Shahidi B, Rangrazi A. The effects of photobiomodulation therapy for treatment of alveolar osteitis (dry socket): systematic review and meta-analysis. Photodiagnosis Photodyn Ther. 2020;32 - PubMed
-
- Dadjoo S, Michelogiannakis D, Rossouw PE, Javed F. Potential adjunct therapies for the management of temporomandibular disorders: an evidence-based review. Cranio. 2022:1–11. - PubMed
-
- Qadri T, Javed F, Johannsen G, Gustafsson A. Role of diode lasers (800-980 nm) as adjuncts to scaling and root planing in the treatment of chronic periodontitis: a systematic review. Photomed Laser Surg. 2015;33:568–575. - PubMed
-
- Onur SG. Evaluation of pain perception and wound healing after laser-assisted frenectomy in pediatric patients: a retrospective comparative study. Photobiomodul Photomed Laser Surg. 2021;39:204–210. - PubMed
-
- Javed F, Kellesarian SV, Romanos GE. Role of diode lasers in oro-facial pain management. J Biol Regul Homeost Agents. 2017;31:153–155. - PubMed
-
- Nejat AH, Eshghpour M, Danaeifar N, Abrishami M, Vahdatinia F, Fekrazad R. Effect of photobiomodulation on the incidence of alveolar osteitis and postoperative pain following mandibular third molar surgery: a double-blind randomized clinical trial. Photochem Photobiol. 2021;97:1129–1135. - PubMed
-
- Jovanović G, Urić N, Krunić N, Tijanić M, Stojanović S. [Assessment of the effectiveness of low level laser in the treatment of alveolar osteitis] Vojnosanit Pregl. 2011;68:506–510. - PubMed
-
- Kaya G, Yapici G, Savaş Z, Güngörmüş M. Comparison of alvogyl, SaliCept patch, and low-level laser therapy in the management of alveolar osteitis. J Oral Maxillofac Surg. 2011;69:1571–1577. - PubMed
-
- Kamal A, Salman B, Ar NH, Samsudin AR. Management of dry socket with low-level laser therapy. Clin Oral Investig. 2021;25:1029–1033. - PubMed
-
- Reed MD, Van Nostran W. Assessing pain intensity with the visual analog scale: a plea for uniformity. J Clin Pharmacol. 2014;54:241–244. - PubMed
-
- Ghosh A, Aggarwal VR, Aetiology Moore R. prevention and management of alveolar osteitis-a scoping review. J Oral Rehabil. 2022;49:103–113. - PubMed
-
- Chen L, Zhu L, Wang K, et al. Antinociceptive effect of prostatic acid phosphatase in a rat model of cancer-induced bone pain. Pain Physician. 2013;16:533–546. - PubMed
-
- Park CK, Li HY, Yeon KY, et al. Eugenol inhibits sodium currents in dental afferent neurons. J Dent Res. 2006;85:900–904. - PubMed
-
- Muñoz-Cámara D, Pardo-Zamora G, Camacho-Alonso F. Postoperative effects of intra-alveolar application of 0.2% chlorhexidine or 1% hyaluronic acid bioadhesive gels after mandibular third molar extraction: a double-blind randomized controlled clinical trial. Clin Oral Investig. 2021;25:617–625. - PubMed
-
- Zhu J, Zhang S, Yuan X, et al. Effect of platelet-rich fibrin on the control of alveolar osteitis, pain, trismus, soft tissue healing, and swelling following mandibular third molar surgery: an updated systematic review and meta-analysis. Int J Oral Maxillofac Surg. 2021;50:398–406. - PubMed
-
- Riba-Terés N, Jorba-García A, Toledano-Serrabona J, Aguilar-Durán L, Figueiredo R, Valmaseda-Castellón E. Microbiota of alveolar osteitis after permanent tooth extractions: a systematic review. J Stomatol Oral Maxillofac Surg. 2021;122:173–181. - PubMed