Early Diagnosis of Classic Homocystinuria in Kuwait through Newborn Screening: A 6-Year Experience
Hind Alsharhan 1 2 3, Amir A Ahmed 4 5, Naser M Ali 5, Ahmad Alahmad 6, Buthaina Albash 3, Reem M Elshafie 3 5, Sumaya Alkanderi 3 5, Usama M Elkazzaz 7, Parakkal Xavier Cyril 8, Rehab M Abdelrahman 4, Alaa A Elmonairy 3, Samia M Ibrahim 9, Yasser M E Elfeky 10, Doaa I Sadik 3, Sara D Al-Enezi 6, Ayman M Salloum 11, Yadav Girish 12, Mohammad Al-Ali 5, Dina G Ramadan 13, Rasha Alsafi 14, May Al-Rushood 4, Laila Bastaki 3
Affiliations
Affiliations
- Department of Pediatrics, Faculty of Medicine, Kuwait University, P.O. Box 24923, Safat 13110, Kuwait.
- Department of Pediatrics, Farwaniya Hospital, Ministry of Health, Sabah Al-Nasser 92426, Kuwait.
- Kuwait Medical Genetics Center, Ministry of Health, Sulaibikhat 80901, Kuwait.
- Newborn Screening Laboratory, Kuwait Medical Genetics Center, Ministry of Health, Sulaibikhat 80901, Kuwait.
- Next Generation Sequencing Laboratory, Kuwait Medical Genetics Center, Ministry of Health, Sulaibikhat 80901, Kuwait.
- Molecular Genetics Laboratory, Kuwait Medical Genetics Center, Ministry of Health, Sulaibikhat 80901, Kuwait.
- Newborn Screening Office, Farwaniya Hospital, Ministry of Health, Sabah Al-Nasser 92426, Kuwait.
- Newborn Screening Office, Adan Hospital, Ministry of Health, Hadiya 52700, Kuwait.
- Newborn Screening Office, Al-Sabah Maternity Hospital, Ministry of Health, Sulaibikhat 80901, Kuwait.
- Newborn Screening Office, Jahra Hospital, Ministry of Health, Jahra 00020, Kuwait.
- Biochemistry Laboratory, Al-Sabah Hospital, Ministry of Health, Shuwaikh 70051, Kuwait.
- Clinical Biochemistry Laboratory, Ibn Sina Hospital, Ministry of Health, Shuwaikh, P.O. Box 25427, Safat 13115, Kuwait.
- Department of Pediatrics, Al-Sabah Hospital, Ministry of Health, Shuweikh 70051, Kuwait.
- Department of Pediatrics, Adan Hospital, Ministry of Health, Hadiya 52700, Kuwait.
Abstract
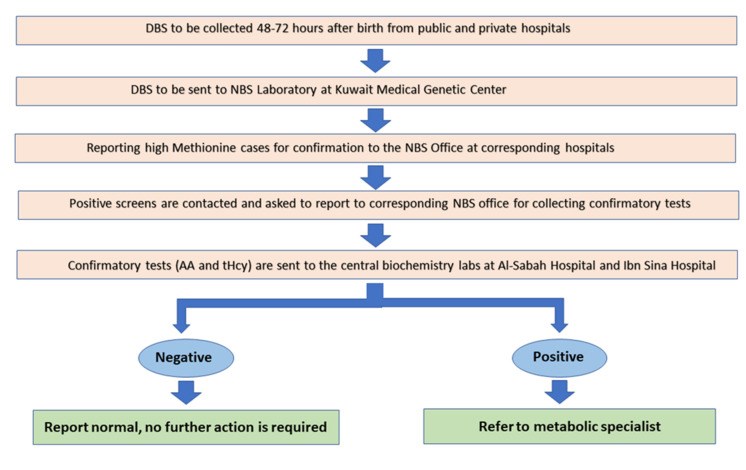
Kuwait is a small Arabian Gulf country with a high rate of consanguinity and where a national newborn screening program was expanded in October 2014 to include a wide range of endocrine and metabolic disorders. A retrospective study conducted between January 2015 and December 2020 revealed a total of 304,086 newborns have been screened in Kuwait. Six newborns were diagnosed with classic homocystinuria with an incidence of 1:50,000, which is not as high as in Qatar but higher than the global incidence. Molecular testing for five of them has revealed three previously reported pathogenic variants in the CBS gene, c.969G>A, p.(Trp323Ter); c.982G>A, p.(Asp328Asn); and the Qatari founder variant c.1006C>T, p.(Arg336Cys). This is the first study to review the screening of newborns in Kuwait for classic homocystinuria, starting with the detection of elevated blood methionine and providing a follow-up strategy for positive results, including plasma total homocysteine and amino acid analyses. Further, we have demonstrated an increase in the specificity of the current newborn screening test for classic homocystinuria by including the methionine to phenylalanine ratio along with the elevated methionine blood levels in first-tier testing. Here, we provide evidence that the newborn screening in Kuwait has led to the early detection of classic homocystinuria cases and enabled the affected individuals to lead active and productive lives.
Keywords: classic homocystinuria; incidence; methionine; molecular testing; newborn screening; total homocysteine.
Conflict of interest statement
The authors declare no conflict of interest.
Figures
Similar articles
Asamoah A, Wei S, Jackson KE, Hersh JH, Levy H.Int J Neonatal Screen. 2021 Jul 23;7(3):48. doi: 10.3390/ijns7030048.PMID: 34449521 Free PMC article.
Gramer G, Abdoh G, Ben-Omran T, Shahbeck N, Ali R, Mahmoud L, Fang-Hoffmann J, Hoffmann GF, Al Rifai H, Okun JG.World J Pediatr. 2017 Apr;13(2):136-143. doi: 10.1007/s12519-017-0003-z. Epub 2017 Jan 15.PMID: 28101774
Gan-Schreier H, Kebbewar M, Fang-Hoffmann J, Wilrich J, Abdoh G, Ben-Omran T, Shahbek N, Bener A, Al Rifai H, Al Khal AL, Lindner M, Zschocke J, Hoffmann GF.J Pediatr. 2010 Mar;156(3):427-32. doi: 10.1016/j.jpeds.2009.09.054. Epub 2009 Nov 14.PMID: 19914636
The Spectrum of Mutations of Homocystinuria in the MENA Region.
Al-Sadeq DW, Nasrallah GK.Genes (Basel). 2020 Mar 20;11(3):330. doi: 10.3390/genes11030330.PMID: 32245022 Free PMC article. Review.
Early Development of Newborn Screening for HCU and Current Challenges.
Levy HL.Int J Neonatal Screen. 2021 Oct 25;7(4):67. doi: 10.3390/ijns7040067.PMID: 34842599 Free PMC article. Review.
Cited by
Bittmann S, Villalon G, Moschuring-Alieva E, Luchter E, Bittmann L.J Clin Med Res. 2023 Feb;15(2):76-83. doi: 10.14740/jocmr4843. Epub 2023 Feb 28.PMID: 36895619 Free PMC article. Review.
Precision information extraction for rare disease epidemiology at scale.
Kariampuzha WZ, Alyea G, Qu S, Sanjak J, Mathé E, Sid E, Chatelaine H, Yadaw A, Xu Y, Zhu Q.J Transl Med. 2023 Feb 28;21(1):157. doi: 10.1186/s12967-023-04011-y.PMID: 36855134 Free PMC article.
Samarasinghe N, Mahaliyanage D, De Silva S, Jasinge E, Punyasiri N, Dilanthi HW.J Genet Eng Biotechnol. 2022 Dec 13;20(1):164. doi: 10.1186/s43141-022-00449-7.PMID: 36512268 Free PMC article.
KMEL References
References
-
- Kuwait Government Online Geography of Kuwait. [(accessed on 14 April 2021)]; Available online: https://www.e.gov.kw/sites/kgoenglish/Pages/Visitors/AboutKuwait/KuwaitA....
-
- Kuwait Government Online Citizens and Residents. [(accessed on 14 April 2021)]; Available online: https://www.e.gov.kw/sites/kgoenglish/Pages/CitizensResidents/citizensAn....
-
- Gan-Schreier H., Kebbewar M., Fang-Hoffmann J., Wilrich J., Abdoh G., Ben-Omran T., Shahbek N., Bener A., Al Rifai H., Al Khal A.L., et al. Newborn Population Screening for Classic Homocystinuria by Determination of Total Homocysteine from Guthrie Cards. J. Pediatr. 2010;156:427–432. doi: 10.1016/j.jpeds.2009.09.054. - DOI - PubMed
-
- Ismail H.M., Krishnamoorthy N., Al-Dewik N., Zayed H., Mohamed N.A., Di Giacomo V., Gupta S., Häberle J., Thöny B., Blom H.J., et al. In silico and in vivo models for Qatari-specific classical homocystinuria as basis for development of novel therapies. Hum. Mutat. 2019;40:230–240. doi: 10.1002/humu.23682. - DOI - PMC - PubMed
-
- Morris A.A.M., Kožich V., Santra S., Andria G., Ben-Omran T.I.M., Chakrapani A.B., Crushell E., Henderson M.J., Hochuli M., Huemer M., et al. Guidelines for the diagnosis and management of cystathionine beta-synthase deficiency. J. Inherit. Metab. Dis. 2017;40:49–74. doi: 10.1007/s10545-016-9979-0. - DOI - PMC - PubMed
-
- Keller R., Chrastina P., Pavlikova M., Gouveia S., Ribes A., Kölker S., Blom H.J., Baumgartner M.R., Bártl J., Dionisi-Vici C., et al. Newborn screening for homocystinurias: Recent recommendations versus current practice. J. Inherit. Metab. Dis. 2019;42:128–139. doi: 10.1002/jimd.12034. - DOI - PubMed
-
- ACT Sheets and Algorithms. [(accessed on 13 April 2021)]; Available online: https://www.acmg.net/ACMG/Medical-Genetics-Practice-Resources/ACT_Sheets....
-
- Schulze A., Lindner M., Kohlmüller D., Olgemöller K., Mayatepek E., Hoffmann G.F. Expanded Newborn Screening for Inborn Errors of Metabolism by Electrospray Ionization-Tandem Mass Spectrometry: Results, Outcome, and Implications. Pediatrics. 2003;111:1399–1406. doi: 10.1542/peds.111.6.1399. - DOI - PubMed
-
- Nexo E., Engbaek F., Ueland P.M., Westby C., O’Gorman P., Johnston C., Kase B.F., Guttormsen A.B., Alfheim I., McPartlin J., et al. Evaluation of Novel Assays in Clinical Chemistry: Quantification of Plasma Total Homocysteine. Clin. Chem. 2000;46:1150–1156. doi: 10.1093/clinchem/46.8.1150. - DOI - PubMed
-
- Bártl J., Chrastina P., Krijt J., Hodík J., Pešková K., Kožich V. Simultaneous determination of cystathionine, total homocysteine, and methionine in dried blood spots by liquid chromatography/tandem mass spectrometry and its utility for the management of patients with homocystinuria. Clin. Chim. Acta. 2014;437:211–217. doi: 10.1016/j.cca.2014.07.028. - DOI - PubMed
-
- Stabler S.P., Korson M., Jethva R., Allen R.H., Kraus J.P., Spector E.B., Wagner C., Mudd S.H. JIMD Reports. Springer; Berlin/Heidelberg, Germany: 2013. Metabolic profiling of total homocysteine and related compounds in hyperho-mocysteinemia: Utility and limitations in diagnosing the cause of puzzling thrombophilia in a family; pp. 149–163. - PMC - PubMed
-
- Okun J.G., Gan-Schreier H., Ben-Omran T., Schmidt K.V., Fang-Hoffmann J., Gramer G., Abdoh G., Shahbeck N., Al Rifai H., Al Khal A.L., et al. JIMD Reports. Springer; Berlin/Heidelberg, Germany: 2016. Newborn Screening for Vitamin B6 Non-responsive Classical Homo-cystinuria: Systematical Evaluation of a Two-Tier Strategy; pp. 87–94. - PMC - PubMed
-
- Hoedt A.E.T., Van Kempen A., Boelen A., Duran M., Kemper-Proper E.A., Oey-Spauwen M.J.W., Wijburg F.A., Bosch A.M. High incidence of hypermethioninaemia in a single neonatal intensive care unit detected by a newly introduced neonatal screening programme. J. Inherit. Metab. Dis. 2007;30:978. doi: 10.1007/s10545-007-0701-0. - DOI - PubMed
-
- Turgeon C.T., Magera M.J., Cuthbert C.D., Loken P.R., Gavrilov D.K., Tortorelli S., Raymond K.M., Oglesbee D., Rinaldo P., Matern D. Determination of Total Homocysteine, Methylmalonic Acid, and 2-Methylcitric Acid in Dried Blood Spots by Tandem Mass Spectrometry. Clin. Chem. 2010;56:1686–1695. doi: 10.1373/clinchem.2010.148957. - DOI - PubMed
-
- Sacharow S.J., Picker J.D., Levy H.L. Homocystinuria Caused by Cystathionine Beta-Synthase Deficiency. In: Adam M.P., Ardinger H.H., Pagon R.A., Wallace S.E., Bean L.J.H., Mirzaa G., Amemiya A., editors. Reviews in GeneReviews® [Internet] University of Washington; Seattle, DC, USA: 2004.
-
- Yap S., Naughten E. Homocystinuria due to cystathionine β-synthase deficiency in Ireland: 25 years’ experience of a newborn screened and treated population with reference to clinical outcome and biochemical control. J. Inherit. Metab. Dis. 1998;21:738–747. doi: 10.1023/A:1005445132327. - DOI - PubMed
-
- Gramer G., Abdoh G., Ben-Omran T., Shahbeck N., Ali R., Mahmoud L., Fang-Hoffmann J., Hoffmann G.F., Al Rifai H., Okun J.G. Newborn screening for remethylation disorders and vitamin B12 deficiency-evaluation of new strategies in cohorts from Qatar and Germany. World J. Pediatr. 2017;13:136–143. doi: 10.1007/s12519-017-0003-z. - DOI - PubMed
-
- Al-Dewik N., Ali A., Mahmoud Y., Shahbeck N., Ali R., Mahmoud L., Al-Mureikhi M., Al-Mesaifri F., Musa S., El-Akouri K., et al. Natural history, with clinical, biochemical, and molecular characterization of classical homocystinuria in the Qatari population. J. Inherit. Metab. Dis. 2019;42:818–830. doi: 10.1002/jimd.12099. - DOI - PubMed
-
- Al-Hammadi M.I. Presentation of Qatari Identity at National Museum of Qatar: Between Imagination and Reality. J. Conserv. Mus. Stud. 2018;16 doi: 10.5334/jcms.171. - DOI
-
- Shibata N., Hasegawa Y., Yamada K., Kobayashi H., Purevsuren J., Yang Y., Dung V.C., Khanh N.N., Verma I.C., Bijarnia-Mahay S., et al. Diversity in the incidence and spectrum of organic acidemias, fatty acid oxidation disorders, and amino acid disorders in Asian countries: Selective screening vs. expanded newborn screening. Mol. Genet. Metab. Rep. 2018;16:5–10. doi: 10.1016/j.ymgmr.2018.05.003. - DOI - PMC - PubMed
-
- Zaidi S., Faiyaz-Ul-Haque M., Shuaib T., Balobaid A., Rahbeeni Z., Abalkhail H., Al-Abdullatif A., Al-Hassnan Z., Peltekova I., Al-Owain M. Clinical and molecular findings of 13 families from Saudi Arabia and a family from Sudan with homocystinuria. Clin. Genet. 2011;81:563–570. doi: 10.1111/j.1399-0004.2011.01690.x. - DOI - PubMed